Oral cavity cancer treatment Worldwide: Best Hospitals, Doctors, Options, & Cost
Oral cavity cancer treatment is a global health problem. There were 600,000+ new cases worldwide annually. The overall survival rate is just 40% to 50% after five years, which hasn't improved much in the last 30 years. Most patients are diagnosed late when the disease is advanced, and oral cavity cancer treatment for stage 3 or 4 is hard. However, concerning the oral cavity cancer treatment prognosis, if oral cancers are found early, the chance of surviving for at least 5 years is 86%. But, only 28% of cancers are discovered at this stage.
Risky behaviors like tobacco and alcohol use, and the growing problem of papillomavirus-related oral cancers, make prevention difficult. Genetic variations also make it hard to find an oral cavity cancer treatment that will work for everyone. That's why the plan to fight the diseases includes early detection and research into the new lip and oral cavity cancer treatment methods.
Best oral cavity cancer treatment clinics
Selecting a hospital for oral cavity cancer
Choosing the right hospital for oral cavity cancer treatment involves careful analysis. A team of specialists, adherence to international guidelines, cutting-edge facilities including robotic surgery, and active clinical research involvement are crucial.
Targeted medicines and immunotherapy, ensuring comprehensive post-operative care with reconstructive surgery and rehabilitation services, and supportive care like psychological support are important for holistic treatment. That is also crucial in choosing a hospital for the oral cavity.
The clinic or center's reputation, location, and treatment costs are critical factors in deciding. The choice of hospital for oral cavity cancer treatment ultimately depends on your needs, requiring thorough research and an understanding of the capabilities of each center.
Top doctors for oral cavity cancer
Advice for oral cavity cancer doctor finding
The selection of an oral cavity cancer doctor involves careful consideration of their specialization, professional affiliations, experience, success rates, approach to care, involvement in research, patient reviews, communication skills, and location. Take your time to research and make an informed choice.
Finding the best doctor for stage 1 oral cavity cancer or for any other stage, you will trust and feel comfortable with that professional, which can significantly improve your treatment journey.
If the process seems overwhelming, remember, AiroMedical is here to assist you. We can provide advice, information, and support to help you find the best oral cavity cancer doctor. Let us help you navigate your journey to recovery.
Top offers
Treatment of oral cavity cancer
The process of oral cavity cancer treatment involves a multi-faceted approach, utilizing several modalities tailored to the patient's condition. The primary oral cavity cancer treatment options include surgery, radiation therapy, immunotherapy, and chemotherapy.
Surgical treatment
In oral cavity, cancer treatment, surgery is often the primary choice, and its kinds and methods depend on the stage and tumor location. The overall survival rate after the initial surgery in connection with the cancer stage was 84% after treatment for stage 1, 71% for stage II, 36% for stage III, and 28% after treatment for stage 4.
This approach can also be highly effective after the treatment for stage 2. For example, the 8-year study reported about 100% disease-specific survival for squamous oral cell cavity carcinoma at its early stages.
The effectiveness of these surgeries is influenced by the cancer's location and stage and the patient's overall health. The survival rate for stage III oral cavity cancer is 36%, and for stage IV, it drops to 28%.
The 5-year survival was 84.8% for robotic surgery patients compared to 80.3% for non-robotic surgery patients. Moreover, TORS ensures improved oral cavity cancer treatment recovery of normal function and pleasing aesthetic results.
The results in the study are: over five years, 67% of patients survived. The rates were 80% for no lymph node cancer, 68% for small, and 54% for larger lymph node cancer.
This advanced approach improves surgical outcomes and enhances the patient's quality of life. It's typically used following major surgeries, playing a key role in patient recovery. The improvement, estimated by patients, is "very good" and can reach more than 80 scores.
In conclusion, oral cavity cancer treatment is a complex, individualized process that involves considering the cancer's stage, location, and the patient's health. It often requires a combination of surgery, radiation, chemotherapy, and immunotherapy to control the disease effectively.
Radiation therapy
Radiation therapy, involving high-energy X-rays or particles, is a powerful tool in oral cavity cancer treatment. It is used as the primary method for smaller cancers or patients unfit for surgery, an adjuvant post-surgery to eliminate any remaining cancer cells, or as a neoadjuvant therapy combined with chemotherapy to shrink larger tumors before surgery.
It's also applied in advanced stages and cases of cancer recurrence. Additionally, radiation combined with chemotherapy, known as chemoradiation, often enhances treatment efficacy, despite increased side effects. Radiation therapy is provided in such forms:
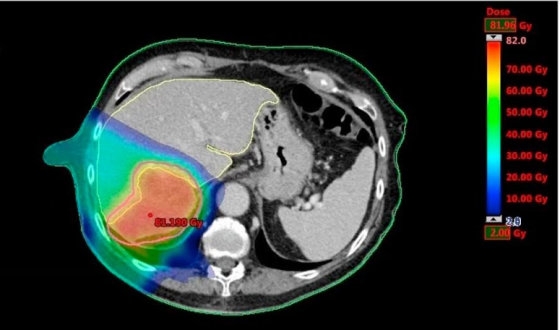
The estimated survival rate for RT alone after 5 years was 22.8% for stages III-IV and 54.2% for stages I-II.
For patients treated with 3D-CRT radiation therapy, the control of local or regional cancer growth was at 79.2%. Their disease-free survival rate was 41.3%, and the overall survival rate was 44.9%.
In patients treated with IMRT radiation therapy, control of local or regional cancer growth was observed in 68.7% of cases. The disease-free survival rate was 48.6%, and the overall survival rate was 55.0%.
This oral cavity cancer treatment success, due to the study, the local control range, depending on the follow-up periods, range from 88 to 100%, disease-free survival from 65 to 96.3%, and overall survival from 94.5 to 98.4%.
After brachytherapy, 79% of patients got fully better, and 21% improved partially. With surgery, 100% of early-stage and 78% of advanced-stage patients saw their condition controlled.
The choice of method often depends on the specific characteristics of the patient's cancer, overall health, and oral cavity cancer treatment goals.
Chemotherapy
Chemotherapy, used alone or in combination with radiation (chemoradiation), can enhance the effectiveness of oral cavity cancer treatment by killing remaining cancer cells post-surgery or making the tumor more susceptible to radiation. It can also be employed in cases where cancer has spread or returned. However, it is rarely used alone for oral cavity cancer treatment.
The researchers say that 66.9% of patients were still alive after five years, and 65.9% were disease-free. As for functionality, the vast majority of patients (92.2%) could eat and maintain their weight without needing a gastric tube.
In addition, treatment following response included chemoradiation, radiation, or surgery, with 40.8% avoiding organ removal. Five-year survival rates were 51.4% overall and 66.9% disease-specific.
Immunotherapy
Immunotherapy is used for oral cavity cancer treatment, leveraging the body's immune system to target and destroy cancer cells. Unlike chemotherapy, immunotherapy involves fewer severe side effects. It acts on specific immune system proteins to enhance their cancer-fighting abilities.
Nivolumab is administered via intravenous infusion every 2 or 4 weeks, while Pembrolizumab is given every 3 or 6 weeks. Pembrolizumab may also be used alone or alongside chemotherapy as a primary treatment for certain patients. Results of this oral cavity cancer treatment are promising: over half of the patients (52%) observed a decrease in the size of their primary tumor following immunotherapy.
Certain immunotherapies, like monoclonal antibodies, serve a dual purpose. They function as targeted drug therapy by inhibiting specific proteins in cancer cells, preventing their growth.
Targeted therapy
Targeted therapy in oral cavity cancer treatment uses drugs like Cetuximab that can be combined with radiation for patients who can't handle the aggressive nature of chemoradiation.
More specific approaches for oral cavity cancer treatment
As we learn more about the unique characteristics of individual patients' cancers, oncology is moving towards more personalized treatments and techniques.
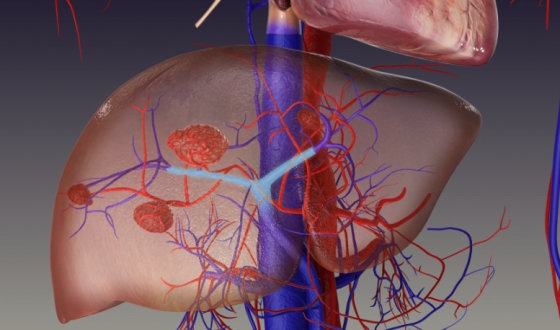
While not yet a standard oral cavity cancer treatment option, it might be considered in select oral cavity cancer cases where conventional surgical approaches are high-risk or unfeasible. Some of the results are reported in the study, under local anesthesia, with no swallow and speech defects and with excellent cosmetic effects.
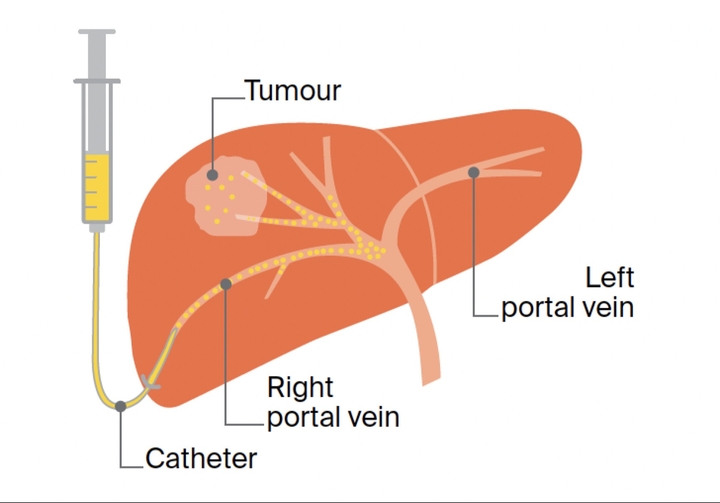
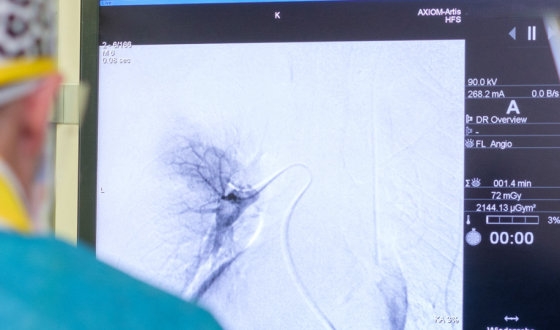
One goal of using embolization, particularly trans-arterial embolization, is to stop bleeding in patients with advanced oral cavity cancer who have bleeding issues during definitive concurrent chemoradiotherapy (CCRT). The effect of bleeding stop is 100%.
Early-phase clinical trials are exploring the use of therapeutic vaccines designed to stimulate an immune response against specific tumor antigens found in individual patients' oral cavity cancers. These are promising results for oral cavity cancer treatment: CAR-T cell therapy has reduced the size of some tumors by 56%, and nearly all cancer cells were killed.
Pain management might involve a combination of medications, nerve blocks, or non-pharmacologic techniques like cognitive-behavioral therapy. Moreover, palliative care teams provide psychological and social support, addressing the comprehensive needs of patients and their families.
For oral cavity cancer treatment, these approaches may offer new hope for patients, particularly those with advanced or recurrent diseases less responsive to standard therapies.
Selection for oral cavity cancer treatment depends on various factors, including the cancer's form and location, the patient's overall health, potential side effects, and personal preferences. Selecting the treatment options for oral cavity and oropharyngeal cancer by stage is a key part of planning. A combination of treatments is often employed to provide the most effective approach. As treatment plans are highly individualized, discussions with the healthcare team are essential to choosing the best action.
Oral cavity cancer treatment cost
Oral cavity cancer€250 - 412,540
Advantages of medical travel
Health tourism, where people travel to another country for medical treatment, is increasingly popular, especially for those with conditions like oral cavity cancer. This trend offers a variety of benefits, including access to advanced therapies, skilled specialists, and high-quality healthcare facilities.
The key benefits of oral cavity cancer treatment abroad
In conclusion, medical travel provides many opportunities for oral cavity cancer treatment, offering patients access to specialized methods that may not be available or affordable in their home country. However, it's crucial for each patient to meticulously research potential destinations and discuss these options with their local healthcare providers to make a well-informed decision that best fits their personal health needs.
Summarizing, every oral cavity cancer treatment option should be considered when facing a diagnosis. Medical tourism provides an important avenue to potentially life-saving treatments, specialists, and advanced technology that might not be available or affordable locally.
With AiroMedical, your journey to better health can be streamlined and supported. We connect you and world-renowned medical facilities, ensuring you receive the best oral cavity cancer treatment as possible. We'll assist with each process step, from choosing the ideal medical destination to coordinating your oral cavity cancer treatment plan and travel logistics. Don't let geographical boundaries limit your treatment options. Reach out to AiroMedical today and explore a world of medical opportunities.
How AiroMedical can help you
Read more in our blogs
FAQ
What are the best clinics for Oral cavity cancer?
Who are the best doctors for Oral cavity cancer?
Prof. Dr. med. Thomas Vogl from
University Hospital Frankfurt am Main
Dr. med. Anett Tillmann, MBA from
Bundeswehr Hospital Berlin
Prof. Dr. med. Roland Ladurner from
Martha-Maria Hospital Munich
Prof. Dr. med. Alexander Muacevic from
European Radiosurgery Centre Munich
Prof. Dr. med. Harald-Robert Bruch, MSc, PhD from
Oncological and Haematological Praxis Clinic Bonn