Transplantology (Organ Transplant) Worldwide: Best Hospitals, Doctors, Options, & Cost
Best transplant centers
A quick guide to selecting a transplant center
Before choosing a transplantology hospital, paying attention to its profile and specialization is necessary. Always look for clinics with many years of proven experience. The number of patients' positive reviews forms the reputation of a hospital. International accreditation and certificates will also help ensure a successful transplant.
The surgery result depends on the frequency of organ transplants you need, the percentage of successful operations and organ rejections, updated equipment, and transplant doctor qualifications. The best transplantology clinics use minimally invasive techniques and develop intensive aftercare programs to increase the chances of long-term functioning of transplanted organs. An important factor is the presence of large donor banks in the country. Thus, patients do not have to wait long for surgery.
AiroMedical lists only proven centers that show the best results. Our experts have compiled transplant hospital rankings for your convenience, which can be found on our platform.
Top-rated transplant doctors
Features of the best transplant specialist
Before choosing which surgeon to contact, ask about the availability of certificates and licenses for such operations and read patients' reviews. Finding a transplant doctor who has been practicing for several years and has the necessary training and experience to provide quality care is essential.
Leading transplantologists work in specialized medical institutions, university clinics, and research institutes. The availability of high-quality, modern equipment gives you an incredible advantage in the issue of organ transplants. The best transplant surgeons usually have different specializations. Therefore, it is worth choosing someone with experience with diseases similar to yours, for example, urologist for kidney transplant.
You can get more information about organ transplant features and find a transplant doctor on the AiroMedical platform. Assess our selection tools to find the right doctor for your case.
What organs are transplanted?
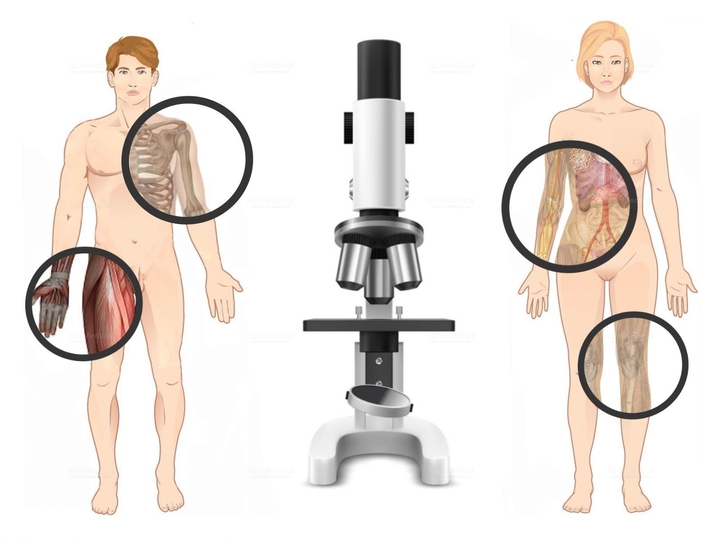
Saving a person's life through organ transplantation is a risky procedure. The new organ needs to be accepted by the immune system, which can be challenging since foreign tissue is often rejected. As a result, not all organs can be successfully transplanted. Some body parts, such as the kidneys, heart, liver, pancreas, lungs, and intestines, are more commonly transplanted. Additionally, tissues like tendons, bones, skin, nerves, veins, heart valves, and cornea can be transplanted.
During the operations, two teams of experienced surgeons work: the first takes the organ from the donor, and the second prepares the patient's body for transplantation. Cardiac surgeons connect the donor organ's vessels with the recipient's veins and arteries with the jeweler's precision.
Sometimes, lungs can be transplanted from a dead donor who has suffered brain death. Alternatively, a living donor can donate the lower right lobe of their lung, and another can donate the lower left lobe, which can be transplanted into the recipient's lungs. In some cases, when the heart is weakened by previous diseases, the heart, and lungs are implanted simultaneously.
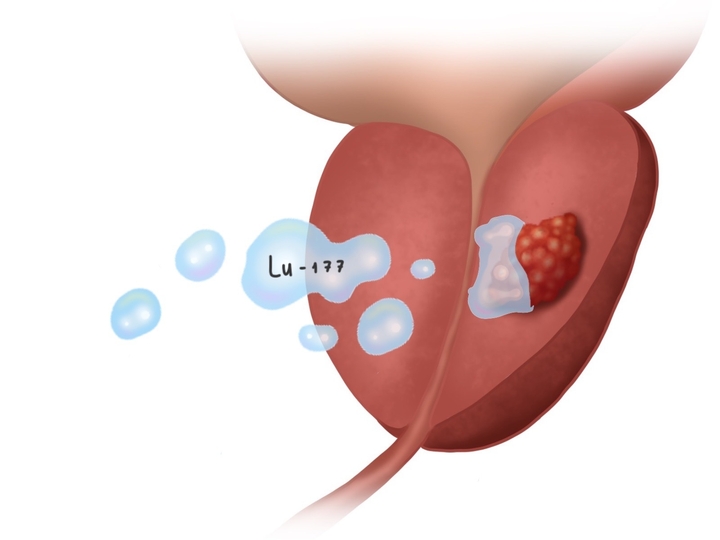
Kidney transplantation has been performed for more than 30 years. Rejection occurs in less than 5% of cases. Highly skilled specialists carry out the procedure in state-of-the-art robotic operating rooms. Minimally invasive surgery is the most common approach, which reduces the recovery period.
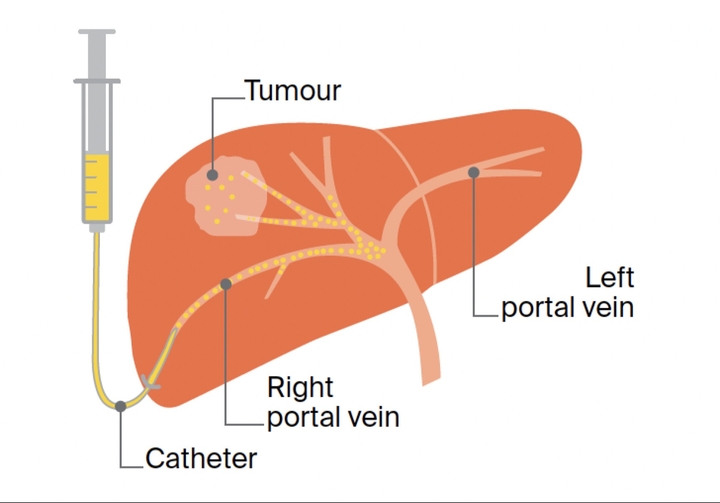
There are several options for transplantation: complete replacement of the affected organ or partial removal of the affected liver area and transplantation of the donor part in its place. The operation takes 8-12 hours. Only 50% can be removed from the donor when donating a liver. However, the patient receiving the transplant needs the entire liver. The success rate for liver transplantation and survival in developed countries is over 95%.
The pancreas is transplanted into the abdominal cavity instead of its original location to minimize the risk of postoperative mortality. The transplant is connected to the iliac, splenic, or hepatic vessels. A catheter is inserted through the abdomen and liver into a vein that supplies the liver during islet transplantation. Donor islet cells are then injected into this vein. If the procedure is successful, the donor cells will produce insulin.
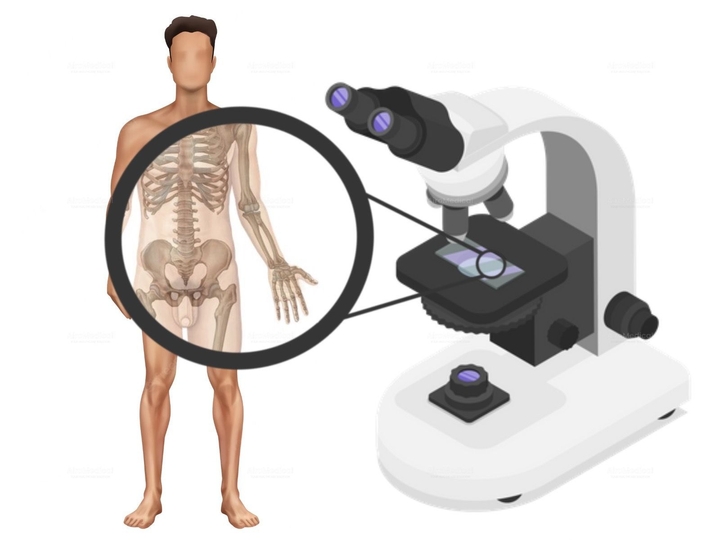
The donor is first stimulated to produce stem cells using specific drugs, which are then collected from their blood and frozen. Next, the patient undergoes chemo- or radiotherapy to eliminate any remaining cancer before receiving the donor bone marrow. After injection, they start to produce new blood cells.
Types of transplant
Transplant surgery in leading centers includes:
Diagnosis before organ transplant
Before surgery, doctors perform various diagnostic procedures to evaluate the patient's physical condition. It's crucial to ensure that the patient is medically fit for transplantation.
The goal is to ensure that the procedure carries an acceptable level of risk for both the patient and the donor. These tests include X-rays, ultrasounds, CT scans, electrocardiograms, echocardiograms, and advanced blood tests that check for underlying illnesses, tumors, and chronic infections.
Types of donor
The importance of a transplant varies depending on the type of organ a person receives. Types of donors:
Most EU countries allow organ and tissue transplantation only from a close relative, which helps to ensure the principles of voluntariness and altruism. Turkey is one of the countries where it is allowed to carry out organ transplantation from a related donor up to the 4th generation (children of second cousins). In addition, family members of the patient's spouse can act as donors. Cross-donation is also available. It is when donors are changed between patients to fit patients according to the parameters necessary for transplantation.
In Italy and other EU states, it is possible to do transplantation with an unrelated donor. However, before proceeding, it is necessary to pass through the ethics committee. This committee ensures that the organ donor is not selling their organ and instead giving it out of pure friendship, altruism, or humanitarian reasons to save the friend or family member's life.
Patient & donor diagnostic process
The doctors evaluate if the patient meets the requirements for surgery. After that, they search for a matching donor and conduct thorough examinations. Specialists consider the age, the general health of the patient and the donor, their weight, age, gender, and organ size. In addition, the donor should not be infected with vector-borne infections such as syphilis, HIV, hepatitis B, and C.
Doctors also conduct compatibility tests:
Step-by-step organ transplant
The surgery differs depending on the donor. For example, suppose an organ is taken from a living person. In that case, it is possible to plan an operation, which is impossible if the organs are obtained from a cadaverous donor who died for unforeseen reasons.
Transplantation process
Every organ has a specific storage limit, and once that limit is exceeded, the organ becomes unsuitable for use. This time varies from organ to organ: heart (4-6 hours), lungs (4-6 hours), liver (12-18 hours), kidneys 48-72 hours, and pancreas (12-24 hours).
Ethical issues, restrictions, & laws by regions
When seeking organ transplantation in foreign countries, it is essential to note that only living-related donors are usually permitted. Furthermore, engaging in any commercial dealings related to organ transplantation is strictly prohibited.
Who can become a donor?
The transplantation of biological tissues and organs is subject to strict regulation at both domestic and international levels. It is primarily to prevent organ trafficking. Patients seeking treatment abroad must comply with legal procedures and obtain all necessary permits. This process is usually quick and runs concurrently with examinations.
World practice
There are two main approaches to posthumous donation worldwide: the presumption of consent and the presumption of disagreement. The first implies that a person a priori agrees to remove his organs in the event of death if there are no written or other indications that he was against it. In the second case, a document confirming his will is required to remove the deceased's organs.
The presumption of consent is in effect in countries such as France, Belgium, Finland, Denmark, Italy, Norway, Sweden, and Spain. Notably, the presumption of consent in the country is not interpreted rigidly; in practice, the last word remains with relatives.
In India and Pakistan, there is a semi-official paid donation. However, the current system may create conflicts of interest between buyers and sellers and prioritize financial gain over compatibility between the donor and recipient. Therefore, it requires revision.
Top offers
Advanced treatment options in transplantology
Transplantology faces two major issues: organ rejection and a shortage of donor organs compared to demand. Researchers are exploring various solutions to overcome these problems in both areas.
Artificial organ transplant
Artificial body parts and their transplantation are becoming increasingly popular, with advancements in polymer materials and medications allowing for the creation of near-perfect replicas of human organs. These include artificial hearts, skin, retinas, and kidneys. The process involves designing the organ, preparing the materials, integrating cells, and allowing the tissues to mature.
However, the main challenge with this technology is that many cells die due to the pressure drop when they exit the printer nozzle. Therefore, it is most suitable for tissues with fewer cells and more connective tissue, like bones and cartilage.
Animal tissues form a matrix or frame to make an artificial organ. The frame is then thoroughly cleaned to remove all protein substances that could cause an immune reaction. Next, cells from the person in need of the organ are placed into the frame, after which the entire workpiece is placed in a bioreactor. Finally, the organ is kept at its usual temperature and environment for several weeks or months until it is fully ready. It is already possible to create a bladder, vagina, urethra, and penis.
After the transplant, no cases of rejection were recorded. At the same time, the genitals were fully functional and allowed a person to have a normal sexual life. Scientists have also created heart valves, trachea, muscles, bones, and cartilage.
The reactor also maintains the proper temperature of the chip and pumps gas into the solution to simulate breathing. These chips have successfully replicated the functions of various organs and tissues, including the liver, kidneys, lungs, adipose tissue, and muscles.
Genetically engineered organs
Operation cost & budget
Organ transplant€37,198 - 340,738
Advantages of medical travel
Transplantation of organs and tissues can be the only solution to save a life. After a successful operation, keeping a close eye on the patient is essential. Top medical centers have organized the process to minimize risks, and in case of complications, patients receive immediate assistance.
Reasons to check transplantation options abroad
At AiroMedical, we use a team approach that puts the patient first. If you have any inquiries about the transplantation process, please don't hesitate to contact us. We're available to provide guidance and help you make an informed choice.
How AiroMedical can help you
Read more in our blogs
FAQ
What are the best clinics for Organ Transplant?
Who are the best doctors for Organ Transplant?
Prof. Dr. med. Jürgen Gschwend from
University Hospital Rechts der Isar Munich
Prof. Dr. med. Helmut Michael Friess from
University Hospital Rechts der Isar Munich
Prof. Dr. med. Jens Werner from
University Hospital Ludwig-Maximilians Munich
Prof. Dr. med. Felix Kyoung-Hwan Chun, MA, FEBU from
University Hospital Frankfurt am Main
Prof. Dr. med. Udo Rolle from
University Hospital Frankfurt am Main