Neuroendocrine (NETs) Tumors Guide

Only about 0,5% of newly diagnosed cancers are neuroendocrine tumors.
12-22% of patients with newly diagnosed neuroendocrine tumors already have metastases.
The prevalence of neuroendocrine tumors in the USA is only 103,312 cases.
There are 2,5 times more female patients with neuroendocrine tumors than male patients.
 What should you know about the neuroendocrine system?
What should you know about the neuroendocrine system?
The neuroendocrine system is represented by organs and cells that combine the properties of nerve cells and cells of the endocrine system. To be more specific, parts of the neuroendocrine system can directly respond to nerve impulses like nerve cells and release hormones, like endocrine cells.
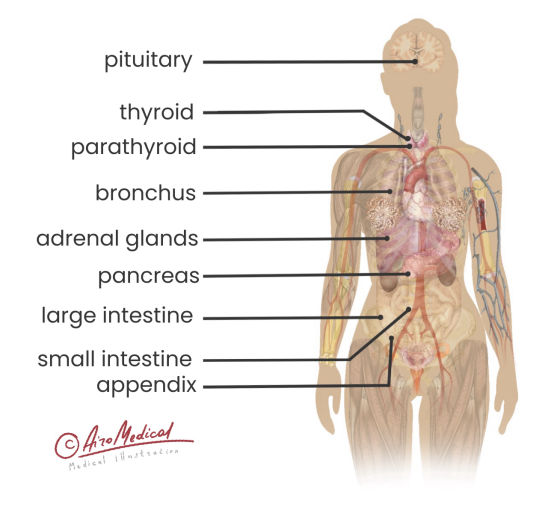
Neuroendocrine cells locate all around the human body, but there are few parts in the brain considering the major centers of neuroendocrine integration. They are the pituitary gland and hypothalamus. Mostly, they control other parts of the neuroendocrine system all over the human body.
Other parts of the neuroendocrine system include:
- Parathyroid glands
- Part of pancreas
- Cells in the breast
- Exocrine cells of the intestine
- Adrenal glands
- Cells in the skin
- Part of thyroid
- Exocrine cells of the respiratory tract
- Part of the urogenital system
The neuroendocrine system plays an essential role in most processes inside the human body. For example, the hypothalamus synthesizes various releasing and inhibiting hormones in response to changes in blood composition and nerve signals. The pituitary gland, in response, starts to increase or decrease the amount of hormone that stimulates other organs of the endocrine system.
As a result, the physiological effect of those hormones on the human body changes accordingly to the released amount of hormone. Organs send slightly different signals (via changing blood composition and nerve impulses) to the hypothalamus. Hypothalamus reacts to those changes by varying the amount of releasing and inhibiting hormones. And these processes make a constant loop that goes around until some links start malfunctioning.
 Neuroendocrine tumors: the basic information
Neuroendocrine tumors: the basic information
Neuroendocrine tumors (NETs) are sporadic (rarely developed) compared to other types of neoplasms. In total, only 2% of all malignancies have signs of neuroendocrine tumors, but only 0,5% are verified as actual NETs.
Due to the specific nature of neuroendocrine cell sites in the human organism, many problems occur when doctors try to create an adequate classification for neuroendocrine tumors. Unfortunately, the neuroendocrine tumor might appear anywhere in the body, but still, some sites are more likely than others.
Among the most widely spread localization of NETs are:
- Intestine (62-67%)
- Lungs (22-27%)
- Pancreas (5-8%)
There are enormous amounts of various neuroendocrine tumors due to a histological type, and nowadays, another classification is mostly used in most clinics. Still, histological features and specifications of every NET are essential for developing the most effective treatment. Generally, all neuroendocrine tumors are separated into two main groups: low-graded (mostly various indolent tumors) and high-graded (mostly highly aggressive carcinomas).
Neuroendocrine tumors might be benign or malignant, but a small number of those tumors didn't show malignant features. Also, up to 40% of neuroendocrine tumors include elements of non-neuroendocrine cells and reveal a diverse nature during examinations via microscope. If the tumor's cells have more than 30% of neuroendocrine components, it is considered a NET.
It's important to know that neuroendocrine tumors can produce various hormones. Still, only 15% of them tend to do it, which is called "functioning." If neuroendocrine tumors don't create hormones, it is often referred to as "non-functional." Yet, in some cases, non-functional NETs can become functional.
 Factors increasing the chances of developing a tumor
Factors increasing the chances of developing a tumor
Generally, doctors didn't discover any significant avoidable factors that could increase or decrease the patient's chances of getting a neuroendocrine tumor. Interestingly, most neuroendocrine tumors are unrelated to environmental aspects, including diet, pollution level, and patients' unhealthy behavior. Among a few exceptions are atypical neuroendocrine tumors of the lungs, which are more likely to develop in smoking patients.
Among the most critical risk factors are the following
- Race/ethnicity. African Americans are more likely to develop gastrointestinal neuroendocrine tumors. Caucasians, in their order, are more likely to get a neuroendocrine tumor in the lung.
- Gender. Women are more likely to develop neuroendocrine tumors than men (2,5:1).
- Age. In most cases, neuroendocrine tumors appear in patients over 60 years and rarely develop in kids.
- Family history. There is a strong relationship between the history of neuroendocrine tumor development among the nearest relatives.
- Certain diseases. Many hereditary diseases are connected with increased chances of getting a NET. Among them are tuberous sclerosis complex, neurofibromatosis type 1, Von Hippel-Lindau syndrome, and many others.
People must understand that they might not develop NETs even if they are already matched, even with several risk factors. Fortunately, there is no 100% correlation between risk factors and neuroendocrine tumor development. Still, it's essential to be aware of potential risks for more effective and attentive regular full-body check-ups and to develop a more informed lifestyle.
Can we prevent neuroendocrine tumors?
Unfortunately, there are no controllable risk factors, and, as a result, there are no effective methods to prevent neuroendocrine tumors.
It's essential to remember that early diagnostics is one of the main factors that make it easier to treat all types of cancer, including neuroendocrine tumors. It will help if you inform your doctor about any possible potential risks.
 What are the main symptoms of NETs?
What are the main symptoms of NETs?
Depending on their localization, histological type, and nature, the disease might show a significant range of symptoms. For example, a neuroendocrine carcinoma in the lungs might lead to a cough (up to 27% of cases), recurrent infectious diseases (up to 49% of cases), and the appearance of blood after a cough (up to 32% of cases). At the same time, if patients got benign neuroendocrine tumors in the lungs, they might remain asymptomatic for a long time.
Still, here are a few of the most common symptoms related to all types of NETs:
- Fatigue. Patients tend to experience fatigue in most cases of neuroendocrine tumors due to the specific nature of treatment and neoplasms.
- Appetite problems. Most often, appetite loss is a system of gastrointestinal neuroendocrine tumors, but it tends to develop when tumors of other sites begin to grow and expand.
- Unexpected weight loss. Weight loss might become especially noticeable in the case of end-stage neuroendocrine cancer, but it's presented more or less in more than 80% of neuroendocrine tumor cases.
Patients with functioning neuroendocrine tumors often develop so-called "carcinoid syndrome." For example, 6-13% of patients with gastrointestinal neuroendocrine tumors develop this syndrome. The ability of such tumors to produce serotonin and hormones causes a range of symptoms, including sweating, face flush, diarrhea, increased heartbeat, and high blood pressure.
Many NET symptoms can vary depending on hormones produced by tumor tissue. For example, if a patient has glucagonoma (a tumor that produces a hormone called glucagon), there is a 29% chance that he will develop stomatitis, gingivitis, and glossitis. Also, there is a 38% chance of getting diabetes. In general, more than 40 types of different functional NETs can lead to various symptoms related to produced hormones.
 How to verify neuroendocrine tumors?
How to verify neuroendocrine tumors?
There are lots of tests that medical practitioners can use to find out if the patient has developed a neuroendocrine tumor. But there is no need to use all of them for each case. For example, to get a full range of necessary information about the features of neuroendocrine tumors, doctors might use the following diagnostic approaches:
- Biopsy. Biopsy remains the only method showing nearly 100% accuracy when verifying neuroendocrine tumors. Pathologists took and examined a small piece of the tumor via microscope. Sometimes, the biopsy is extremely hard to perform due to a site of lesions.
- Medical imaging. Various medical imaging methods proved to be valuable in discovering neuroendocrine tumors. For example, MRI shows about 76% of sensitivity rate, CT - 71%, and PET - up to 95%. Also, it's essential to use various contrasting substances to increase the sensitivity of these methods.
- Endoscopy. A thin, flexible tube is inserted inside the patient's body to get a clear view of lesions during endoscopy. Also, endoscopy can help doctors to take a piece of the tumor for further biopsy.
- Tumor biomarker tests. Those tests help determine specific neuroendocrine tumor features (genes, proteins, etc.).
- Urine or blood lab tests. One of the most effective and easy-to-perform methods to discover abnormal levels of specific proteins and other substances is urine or blood lab tests. Their results shouldn't consider confirmation of neuroendocrine tumors but could give valuable info about the patient's health and further diagnostic steps.
In case a functional NET diagnosis is suspected, it's also essential to check the level of various hormones (including insulin, somatostatin, and glucagon). The result of those lab tests is a valuable source for further clinical research by medical practitioners. Still, they can't consider it a direct confirmation of the NET diagnosis, but it can point them in the right direction.
Staging and grading of neuroendocrine tumors
When grading neuroendocrine tumors, doctors always look for two leading indicators: the number of mitotic (cells that are about to divide soon or undergoing dividing) cells in one view of the microscope and the so-called Ki-67 index, which could be measured during an additional lab test.
According to these indicators, there are the following grades of neuroendocrine tumors
- Grade I. Ki-76 index - <3%, mitotic cells count - <2. Most often, grade 1 neuroendocrine tumors grow very slowly.
- Grade II. Ki-76 index - 3 - 20%, mitotic cells count - 2 to 20. Grade 2 neuroendocrine tumors grow faster and show a slight tendency to develop metastases.
- Grade III. Ki-76 index - >20%, mitotic cells count - >20. Grade 3 neuroendocrine tumors grow very fast and, as a result, often show a tendency to develop metastases.
NETs stages
Every type of neuroendocrine tumor has a slightly varying approach to staging, mainly related to the primary site. However, in most cases, the stage is set according to the TNM system.
- T stands for "tumor" and displays a volume and size of a primary tumor.
- N stands for "nodes" and represents a condition of the nearest lymphatic nodes.
- M stands for "metastases" and gives information about the number and prevalence of metastatic lesions.
As a result, there are four stages for each type of NET, each with different diagnostic approaches and criteria.
The grade of neuroendocrine tumors is most often different from the stage. For example, neuroendocrine cancer stage 4 with metastatic lesions all over the body could potentially be grade 3 or even grade 2. As a result, neuroendocrine tumors of a 3-4 stage could be treated with different approaches due to varying grades. To develop a proper treatment program, doctors need to consider the stage and the grade of NET. So, verifying the NET diagnosis in a reliable hospital is necessary to get as much valuable information about the tumor as possible.
Where are the best countries to treat neuroendocrine tumors?
 What are traditional neuroendocrine tumor treatment options?
What are traditional neuroendocrine tumor treatment options?
The most effective treatment of neuroendocrine tumors is strongly related to their histological type, localization, patients' state, staging, and grading. For example, to treat neuroendocrine tumors of the rectum, most surgeons prefer to use transanal endoscopic microsurgery if possible, which helps to achieve a 5-year survival rate of 99,3%. Unfortunately, it is possible to use this method only if the tumor's size is less than 2 cm.
The most popular approaches to neuroendocrine tumor treatment
Surgery removal techniques. Patients with neuroendocrine lumps often undergo surgical treatment. Mostly, patients with no distant metastases, relatively small tumors, and clean lymphatic nodes are the best suited for surgical removal techniques.
- Open surgery. Surgeons create a big approach to reaching the tumor, and as a result, they might discover some additional details about cancer (e.g., the development of unnoticed metastases). However, open surgeries are often associated with an increased risk of side effects.
- Endoscopic surgery. Surgeons use small cameras to perform endoscopic surgical treatment. Cameras and surgical instruments are inserted through small holes over the lesions. Up to 72% of endoscopic surgeries with neuroendocrine tumors below 20 mm become successful.
Hormonal therapy. Patients with functional NETs might often experience additional negative symptoms due to extra hormones produced by the tumor. In that case, they might get hormonal treatment to suppress those symptoms. For example, somatostatin showed 58-67% efficiency as a treatment for insulinoma (a pancreatic neuroendocrine tumor that produces excess insulin).
Chemotherapy. Chemotherapy could help suppress the growth and spread of cancer cells around the body. Up to 43% of mixed NENs showed a reasonable response rate during chemotherapy.
- Dactolisib. This is one of the advanced substances used for the chemotherapy of cancer patients and often became a part of gastric neuroendocrine tumor treatment complex. It is very effective but pretty toxic. Unfortunately, about 83,9% of patients treated with Dactilisib report adverse side effects.
Immunotherapy. Oncologists often use various methods of immunotherapy to help the patient's immune system fight cancer. Unfortunately, only 11% of neuroendocrine tumors responded to traditional immunotherapy methods.
Targeted therapy. Targeted therapy usually targets various proteins or other substances essential for the growth and development of tumor cells and brakes their supply. Unfortunately, about 10% of NETs respond during the traditional targeted therapy.
Radiation therapy. Radiation therapy mainly uses in addition to surgery, especially in cases when surgeons can't remove a whole neuroendocrine tumor. Often, traditional radiation therapy is used as palliative care for patients with NETs that develop metastases.
Also, due to the ability of these lumps to produce various hormones and specific localization, treatment for neuroendocrine tumors should try to stick to organ-saving patterns. For example, if doctors remove a giant tumor of the hypothalamus or pituitary gland during surgery, there would be no possibility of saving a sufficient amount of those organs' tissues for the organism to produce an adequate amount of certain hormones.
The so-called combined treatment is one of the best metastatic neuroendocrine tumor treatment methods. Combined treatment helps to achieve 30% better tumor management results compared with a single-method therapy. However, achieving the maximum possible treatment effectiveness requires a multidisciplinary approach, including surgeons, oncologists, chemotherapists, and other medical practitioners. A distant medical consultation might help develop the best treatment plan.
Top neuroendocrine tumor treatment centers
 New treatment for neuroendocrine cancer
New treatment for neuroendocrine cancer
Every day, more and more new treatment approaches and methods spread all over the globe. Still, it takes time, money, and effort to make those treatment methods available everywhere. For example, medical practitioners should take some time to get familiar with and learn them. Additional medical supplies and apparatuses need to be both, etc.
Unfortunately, patients with neuroendocrine tumors often receive those treatment options only in clinics and hospitals abroad. Among the most promising new methods of treatment for neuroendocrine cancer are:
Peptide receptor radionuclide therapy (PRRT) with Lu-177. PRRT uses specific radiopharmaceuticals to deliver treatment agents by bounding them with tumor cells, such as Lutetium 177 therapy. Up to 68% of patients with NETs reported an overall improvement in their well-being after PRRT treatment.
Radiofrequency ablation (RFA). During RFA, a massive part of nerves and sometimes vessels that feed tumors are destroyed by the heat generated by AC. In case of successful treatment, studies report no relapses during the following 60 months.
New targeted options. Doctors continue studying neuroendocrine cells and invent more specific approaches to stop cancer growth:
- Sunitinib. This chemical substance represents a new way of molecular targeted therapy, but it still requires improvements. Sunitinib showed efficiency only for 24,5% of patients with G1 or G2 pancreatic NETs.
- mTOR inhibitors. One of the crucial proteins inside most neuroendocrine tumors is the so-called mTOR. It plays a vital role in some tumor cells' physiological processes. Inhibition of mTOR production might help patients with NETs and certain neurological diseases (e.g., Alzheimer's) improve their quality of life and increase life expectancy.
- Cytotoxic T-lymphocyte antigen-4 (CTL4) blockers. CTL4 is a regulator that plays an essential role in the human immune system during tumor response reactions. For now, doctors actively study CTL4 blockers' effects on NETs, but they have shown excellent results in treating patients with melanoma.
Also, many neuroendocrine treatment methods are undergoing clinical trials right now. Those methods might grant a cure to thousands of patients worldwide. AiroMedical could help patients that seek new treatment options and experimental possibilities to become a part of those clinical trials. Still, it's better first to find out more about widely available treatment options.
Top neuroendocrine cancer doctors worldwide
 The prognosis for patients with neuroendocrine tumors
The prognosis for patients with neuroendocrine tumors
It's unclear what kind of prognosis most patients with NETs might get. Sometimes, stage 4 neuroendocrine cancer life expectancy could be pretty long-lasting. For example, patients with stage IV well-differentiated mid-gut neuroendocrine tumors with metastasis have over 75% of a 5-year survival rate.
At the same time, pituitary neuroendocrine carcinoma stage 4 could kill the patient in about eight months. Also, tumor grade plays a crucial role in terms of overall survival.
Overall survival rate depending on neuroendocrine tumor's grade
- Grade I - 16,2 years
- Grade II - 8,3 years
- Grade III - 0,8 year
It's important to remember that most patients with NETs are old (60+ years old), so they might die for other reasons. In any case, the answer to the question: "Can neuroendocrine cancer be cured?" is 100% affirmative. Still, it's necessary to learn about the best available treatment options and get the opinions of the best industry leaders before starting a treatment. AiroMedical will gladly help you contact the best specialist around the globe to get all the necessary information regarding treatment options and offer you complete procedural management during treatment.
References:
- Oronsky B, Ma PC, Morgensztern D, Carter CA. Nothing But NET: A Review of Neuroendocrine Tumors and Carcinomas. Neoplasia. 2017;19(12):991-1002. doi:10.1016/j.neo.2017.09.002
- Kiesewetter B, Raderer M. How I treat neuroendocrine tumors. ESMO Open. 2020;5(4):e000811. doi:10.1136/esmoopen-2020-000811
- Hofland J, Kaltsas G, de Herder WW. Advances in the Diagnosis and Management of Well-Differentiated Neuroendocrine Neoplasms. Endocr Rev. 2020;41(2):371-403. doi:10.1210/endrev/bnz004
- Raphael MJ, Chan DL, Law C, Singh S. Principles of diagnosis and management of neuroendocrine tumors. CMAJ. 2017;189(10):E398-E404. doi:10.1503/cmaj.160771
- Onaitis MW, Kirshbom PM, Hayward TZ, et al. Gastrointestinal carcinoids: characterization by the site of origin and hormone production. Ann Surg. 2000;232(4):549-556. doi:10.1097/00000658-200010000-00010
- Das S, Dasari A. Epidemiology, Incidence, and Prevalence of Neuroendocrine Neoplasms: Are There Global Differences?. Curr Oncol Rep. 2021;23(4):43. Published 2021 Mar 14. doi:10.1007/s11912-021-01029-7
- Kaderli RM, Spanjol M, Kollár A, et al. Therapeutic Options for Neuroendocrine Tumors: A Systematic Review and Network Meta-analysis. JAMA Oncol. 2019;5(4):480-489. doi:10.1001/jamaoncol.2018.6720