Parkinson's Disease (PD) Guide

More people will get Parkinson's, with a 17% increase by 2030.
Parkinson's is primarily diagnosed in those over 60 but can occur as early as 30.
Parkinson's disease affects an estimated 7 million to 10 million people worldwide.
PD is predicted to affect 1% of the global population aged 60+.
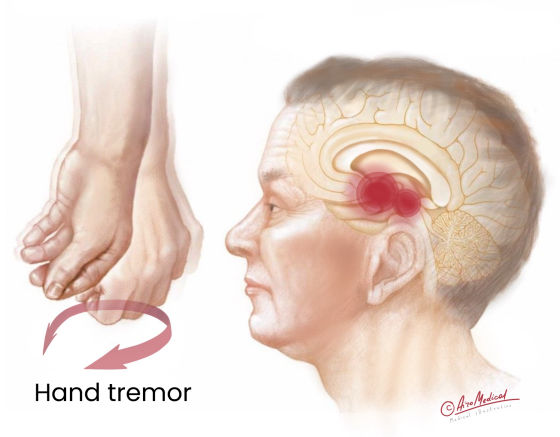
 Some info about where Parkinson’s disease develop
Some info about where Parkinson’s disease develop
Here are some zones in the brain that get involved in Parkinson’s disease.
- The substantia nigra is a region in the midbrain of the brain that plays an essential role in controlling movement. In simple terms, it produces dopamine, which helps transmit signals between nerve cells. These signals are necessary for coordinating activities and maintaining muscle tone. Parkinson's disease causes cells in the substantia nigra that make dopamine break down and die, which lowers the amount of dopamine in the brain.
- The basal ganglia are a group of nuclei in the brain that play a crucial role in controlling movement and coordinating voluntary actions. In the case of PD, the basal ganglia has trouble controlling movement, leading to the disease's main symptoms.
- The thalamus is a central part of the brain that plays a crucial role in processing and relaying sensory information. It acts as a "relay station" for incoming sensory information, receiving signals from the senses (such as sight, touch, and sound) and forwarding them to the appropriate areas of the cerebral cortex for further processing. The thalamus also plays a role in regulating consciousness, sleep, and alertness. In PD development, the thalamus may also be affected, making it hard to control pain and causing sleep problems like insomnia and feeling too sleepy.
- The corpus callosum is a broad bundle of nerve fibers connecting the brain's two hemispheres. It plays a crucial role in communication and coordination. The corpus callosum allows the hemispheres to exchange information and work together as a single, integrated system. It will enable us to use both sides of our brains in a complementary manner.
For example, the right hemisphere is often associated with creativity, and holistic thinking, while the left hemisphere is typically associated with logical thinking and language processing. These two hemispheres can work together through the corpus callosum to solve problems, understand language, and perform other complex tasks.
Cognitive issues like memory loss and trouble-solving difficulties may be caused by changes in the corpus callosum when Parkinson's develops.
 What is Parkinson's disease?
What is Parkinson's disease?
It is a nervous system disorder that makes it hard to move and coordinate. The disease happens when neurons that produce dopamine die off. The condition can affect different brain parts in different ways.
 In addition, people with PD have lost nerve endings that produce a norepinephrine chemical. This chemical helps control heart rate, blood pressure, and other body functions. When not made, it can cause fatigue and problems with blood pressure, digestion, and a sudden drop in blood pressure when transitioning from sitting to standing.
In addition, people with PD have lost nerve endings that produce a norepinephrine chemical. This chemical helps control heart rate, blood pressure, and other body functions. When not made, it can cause fatigue and problems with blood pressure, digestion, and a sudden drop in blood pressure when transitioning from sitting to standing.
There are several forms depending on what causes Parkinson's disease
- Idiopathic: Most people have it, meaning the cause is unknown. The most common symptoms of idiopathic Parkinson's disease are tremors, rigidity, and slow movements.
- Vascular: It is also called the arteriosclerotic kind, which occurs when the blood flow to the brain is cut off. It can sometimes happen to people who have had a mild stroke. Common symptoms include problems with memory, sleep, mood, and movement.
- Drug-induced: It happens when the patient is treated with drugs that affect the dopamine-produced brain’s areas. Neuroleptic medications used to treat schizophrenia and other psychotic disorders stop dopamine from working in the brain. It is the most common cause of drug-induced parkinsonism. Most of the time, their symptoms stay the same. Only very rarely do they get worse.
Other forms of the condition are Parkinson's Plus Syndromes. This group of disorders is characterized by symptoms similar to PD but with additional issues such as dementia, ataxia (uncoordinated movement), or difficulty with eye movements. Some examples include multiple system atrophy and progressive supranuclear palsy.
 What are the risk factors of Parkinson's disease?
What are the risk factors of Parkinson's disease?
The exact cause is not known. Still, it's believed to be a combination of genetics, environment, and other factors. Roughly 10 to 20% of cases are linked to genetic causes. The rest are idiopathic, meaning unknown.
- Age, with the average age of onset being 60;
- Sex: men are 1,5 times more likely to develop the disease.
- Genetic: Individuals with a parent or sibling with Parkinson's also have a higher risk.
- Exposure to environmental toxins: Pesticides, herbicides, heavy metals, detergents, and solvents, are believed to be possible triggers.
Additionally, repeated head trauma, such as boxers might experience, may increase the risk of developing Parkinsonism. Still, more research is needed to confirm this.
Can anyone prevent Parkinson's disease?
Unfortunately, there is no known way to avoid it. However, we can maintain a healthy lifestyle: by eating a balanced diet, do exercise regularly, and avoiding exposure to toxins. These measures may reduce the risk. Additionally, keeping the brain active through reading, playing games, and learning new skills can help. It is also essential to discuss any family history cases with a doctor. It can help identify any potential genetic risk factors. While anyone does not know the cause and can't prevent this life-long illness, early diagnosis and treatment of Parkinson's disease can help manage symptoms and increase the quality of life.
Regular check-ups can be crucial in detecting early signs of Parkinson's disease and managing its symptoms. While there is no known treatment for Parkinson's, early detection and treatment can improve quality of life and slow the progression of the disease.
 Signs and symptoms of Parkinson’s disease
Signs and symptoms of Parkinson’s disease
They typically develop gradually over time and can include the following:
- Tremors: Uncontrollable shaking or trembling, usually starting in the hand or limb.
- Rigidity: Stiffness or resistance to movement in the limbs and trunk.
- Bradykinesia: Slowness of movement, making everyday tasks difficult.
- Postural instability: Difficulty maintaining balance and an increased risk of falling.
- Speech changes: Soft or slurred speech and difficulty with swallowing.
- Writing changes: Smaller or cramped handwriting, known as micrographia.
- Loss of automatic movements: Decreased arm swing, facial expressions, and blinking.
- Fatigue: Tiredness and increased drowsiness.
- Dementia: Progressive decline in memory and thinking abilities.
It is important to note that not all individuals with Parkinson's disease will experience all these symptoms, which may vary in intensity and frequency. Symptoms may also differ from person to person, making early diagnosis and treatment necessary for managing the disease effectively.
 Diagnostic tests
Diagnostic tests
Parkinson's disease is a clinically diagnosed condition. So, neurologists conduct a medical history and physical examination to interpret it. This involves a detailed account of symptoms, medical conditions, medications, family history, and lifestyle factors.
During a neurological examination, the neurologist assesses arm and leg agility, muscle tone, gait, balance, and animation in expression and speech. The presence of tremors, stiffness in extremities or neck, changes in walking, step size, ability to turn, balance, and posture are also evaluated. Some medical conditions and medications may cause similar symptoms. Its severity depends on the Parkinson's stages.
No single laboratory test or imaging study can definitively diagnose this condition. However, specific tests can aid in confirming a diagnosis of PD or excluding other health issues.
These tests may include the following
- Blood tests exclude various forms of parkinsonism.
- A computed tomography (CT) scan uses X-rays and computer technology to create a 3D nervous system image.
- A magnetic resonance imaging (MRI) scan uses a magnet, radio waves, and a computer to produce a clear image of the inside of the body.
- A positron emission tomography (PET) scan involves an injectable radioactive tracer to detect diseased cells and creates 3D images for a more accurate diagnosis.
- Genetic testing to examine blood or bodily fluids for abnormal chromosomes.
- A spinal tap in which a doctor takes a sample of the cerebrospinal fluid surrounding the brain and spinal cord using a thin needle.
- A biopsy involves collecting a small skin sample, including nerves, to determine if specific changes increase the risk of developing the illness.
PD diagnosing can be time-consuming, and regular follow-up visits with movement disorder specialists are often recommended to evaluate the condition and symptoms over time. A definitive diagnosis can be made through ongoing monitoring.
Stages of Parkinson’s disease
These are typically classified into five stages based on the severity and progression of symptoms, as follows:
- Stage 1: Mild symptoms on one side of the body, usually with minimal functional impairment;
- Stage 2: Symptoms begin to affect both sides of the body, with minimal or no balance impairment;
- Stage 3: Balance impairment and slowed movements become more noticeable, but the person can still perform daily tasks independently;
- Stage 4: Symptoms become more severe and disabling, with difficulty walking and standing without assistance;
- Stage 5: The most advanced of Parkinson's disease stages. The person typically cannot stand or walk without assistance and may require full-time care.
Parkinson's can be hard to diagnose, so it is good to regularly see a neurologist trained in movement disorders. It lets the symptoms be watched over time, which makes it easier to make a correct diagnosis.
Which countries offer the latest Parkinson's disease treatment?
 Conventional treatment for Parkinson's disease
Conventional treatment for Parkinson's disease
Medications are a common treatment approach and can help alleviate motor symptoms such as tremors, stiffness, and slow movement.
There are several medications commonly used as treatment options for Parkinson's disease. S
Some of the most frequently prescribed include
- Levodopa is a medication converted into dopamine in the brain, helping alleviate motor symptoms such as tremors, stiffness, and slow movement.
- Dopamine agonists are Parkinson's disease treatment medications that mimic the effects of dopamine in the brain. They can be used alone or in combination with levodopa to manage symptoms.
- MAO-B inhibitors increase dopamine levels in the brain by blocking the activity of an enzyme called monoamine oxidase B.
- COMT inhibitors help prolong levodopa’s effects by preventing it from being broken down too quickly.
- Anticholinergic can help alleviate tremors and other motor symptoms by blocking the activity of a neurotransmitter called acetylcholine.
- Amantadine is a medication that can help reduce dyskinesia and involuntary movements, which can be a side effect of levodopa treatment.
The drugs used for treatment vary depending on the individual and their unique symptoms and needs. However, medications may not be effective for all patients, and ongoing research aims to develop new and more effective treatments for Parkinson's disease.
It also can be treated in several ways that don't involve taking medicine.
Doctors use
- Exercise: Regular physical activity can help improve balance, flexibility, and overall mobility.
- Physical therapy: A physical therapist can give specific exercises and stretches to help with the symptoms.
- Speech therapy to support people with PD who have trouble speaking or swallowing.
- Occupational therapy can help patients find ways to keep doing daily tasks on their own.
- Cognitive behavioral therapy can help people with PD deal with depression, anxiety, and other emotional symptoms.
According to estimates from the Parkinson's Foundation, approximately 1% of people over the age of 60 have Parkinson's disease. While not all require rehabilitation, many will benefit from it during their disease course.
Rehabilitation for Parkinson's disease can help
- Improve mobility increasing their ability to walk, stand, and move around.
- Increase strength, maintain their independence, and perform daily activities.
- Maintain better balance reducing the risk of falls.
- Enhance coordination focusing on coordination and motor skills to improve overall movement patterns and reduce tremors.
- Improve the quality of life to feel more confident and empowered, which can positively impact their overall well-being.
What hospitals are recommended to treat Parkinson's disease?
 New treatment for Parkinson's disease
New treatment for Parkinson's disease
While medications such as Levodopa and therapeutic approach can help manage symptoms, researchers are constantly exploring new treatment options to improve patient outcomes.
Latest surgical treatments for PD
Surgery for Parkinson's disease is not considered a first-line treatment option. The specific criteria for selecting a candidate may vary depending on the type of surgery planned, but here are some general factors:
- Age: While there is no strict age limit, younger patients may be better candidates as they tend to have a longer life expectancy and may benefit more from the procedure.
- Disease duration: Individuals who have had Parkinson's disease for several years may be more likely to experience complications from the surgery.
- Motor symptoms: Surgery is typically considered for individuals with significant motor symptoms that are not well controlled with medication.
- Cognitive function: Candidates for surgery should have a relatively intact cognitive function, as surgery may be associated with mental changes.
- Absence of significant comorbidities: Candidates for surgery should have no significant medical problems that would make surgery riskier.
One promising option is deep brain stimulation (DBS), a surgical treatment for Parkinson's disease that involves implanting a device to deliver electrical current to specific brain areas to stimulate malfunctioning neurons. This treatment is typically used in the later stages of the disease when medications are no longer effective. The research found that stimulation had a lasting effect, cutting motor symptoms by 39% and all of the main signs like tremors, slow movement, stiffness, unstable posture, and trouble walking. Also, there was a significant improvement in activities of daily living.
Another surgical option is MRI-guided focused ultrasound ablation, which uses ultrasound waves to heat and destroy targeted areas of the brain that are responsible for tremors in Parkinson’s. It is a less invasive procedure considered safer than traditional brain surgery.
Non-surgical treatments for Parkinson’s
Stem cell therapy is also being investigated as a potential treatment for PD. Stem cell treatment treats Parkinson's. It replaces damaged brain cells with stem cells, which can become specialized ones. The IV-injected stem cells "home" to damaged and inflamed regions. Stem cells mainly reduce brain tissue inflammation and prevent disease progression by altering the immune system. Stem cell treatment reduces motor symptoms like tremors, stiffness, and difficulty moving by restoring dopamine-producing brain cells.
Finally, gene therapy and gene-targeting treatments are being developed to target mutations that cause Parkinson's disease. Some of these treatments may also improve the effectiveness of medications like Levodopa and boost patient benefits.
While these treatments show promise, they are not widely available and are still being studied. Long-term treatment is often necessary to manage symptoms, and patients may need to adapt to new ways of doing everyday tasks over time. However, ongoing research offers hope for better treatment options in the future.
Who are the best specialists in Parkinson's disease?
 Prognosis and stats for Parkinson’s disease
Prognosis and stats for Parkinson’s disease
Parkinson's disease can cause someone to die and change their life for the worse. When there are other signs of the disease, it becomes dangerous. It can cause people to fall, leading to broken bones, traumatic brain injuries, or even worse, problems. When a patient has injuries and issues, it can shorten their life by a lot.
This latest study examines North American Parkinson's prevalence the most. It counts cases from five epidemiological cohorts since 2012. Smaller studies estimated 40,000–60,000 new PD cases per year. The new rate is nearly 90,000 instances per year, 1.5 times higher. The number of people with PD rises with the number of older people because age is the most significant risk factor.
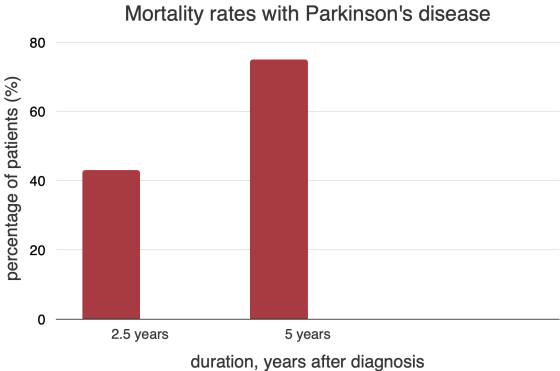
Researchers investigated the effect of Parkinsonism on life expectancy using the Health Improvement Network (THIN), the UK's primary healthcare database with over 12 million electronic health records. The study compared survival rates of individuals with PD up to five years after diagnosis. The results showed that mortality rates increased from 43% within 2.5 years of symptom onset to 75% over the next 2.5 years.
Parkinson's disease and its symptoms are not something anyone has to deal with on their own, which is a good thing. You can get help, support, and advice with just one click. AiroMedical specialists, who know everything there is to know about diseases that affect the nervous system and neurosurgery, collaborate with the finest clinics and doctors to figure out how to treat a patient with Parkinson's disease in the best way possible.
References:
- Miyasaki JM. Treatment of Advanced Parkinson’s Disease and Related Disorders. Continuum (Minneap Minn). 2016 Aug;22 (4 Movement Disorders):1104-16. doi: 10.1212/CON.0000000000000347. PMID: 27495200.
- Thomsen, B.L.C., Jensen, S.R., Clausen, A., Karlsborg, M., Jespersen, B., & Løkkegaard, A. Deep Brain Stimulation in Parkinson's Disease: Still Effective After More Than 8 Years. Movement Disorders Clinical Practice, (2020), 7(7), 788-796. doi: 10.1002/mdc3.13040. PMID: 33033736. PMCID: PMC7534016.
- Willis, A.W., Roberts, E., Beck, J.C., Fiske, B., Ross, W., Savica, R., Van Den Eeden, S.K., Tanner, C.M., & Marras, C. (2022). Incidence of Parkinson’s disease in North America. NPJ, (2022), 8, 170. doi: 10.1038/s41531-022-0166-4.
- Charidimou, A., Seamons, J., Selai, C., & Schrag, A. (2011). The Role of Cognitive-Behavioural Therapy for Patients with Depression in Parkinson's Disease, Published online 2011, 737523. doi: 10.4061/2011/737523.
- Venkataramana, N. K., Kumar, S. K. V., Balaraju, S., Radhakrishnan, R. C., Bansal, A., Dixit, A., Rao, D. K., Das, M., Jan, M., Gupta, P. K., & Totey, S. M. (Open-labeled study of unilateral autologous bone-marrow-derived mesenchymal stem cell transplantation in Parkinson's disease), Science direct, (2012), 658469. doi: 10.1155/2012/658469
- González-Rodríguez, P., Zampese, E., Stout, K.A., Guzman, J.N., Ilijic, E., Yang, B., Tkatch, T., Stavarache, M.A., Wokosin, D.L., Gao, L., Kaplitt, M.G., López-Barneo, J., Schumacker, P.T., & Surmeier, D.J. Disruption of mitochondrial complex, induces progressive parkinsonism. Nature, (2021), 599, 650-656.
- Okunoye O, Horsfall L, Marston L, Walters K, Schrag A. Mortality of People with Parkinson’s Disease in a Large UK-Based Cohort Study: Time Trends and Relationship to Disease Duration. Mov Disord. (2021), Dec 1;36(12):2811-2820. doi: 10.1002/mds.28727. PMID: 34351000; PMCID: PMC7612920.