Retinitis Pigmentosa (RP) Guide

1 in every 4,000 people is affected with retinitis pigmentosa.
Every second patient with retinitis pigmentosa has no family history with it.
Retinitis pigmentosa is caused by harmful changes in more than 50 genes.
If nothing is done, the person with retinitis pigmentosa can lose their vision by age 40. But total blindness is rare.
 Briefly about the vision
Briefly about the vision
The retina, a vital part of our visual system, is a thin layer of tissue at the back of the eye. It contains specialized cells called photoreceptors. There are two kinds of them: rods and cones. They collaborate to transform light into electrical signals for the brain through the optic nerve. Rods facilitate low-light vision and motion detection, while cones allow us to perceive color and details. These cells unite to endow us with the gift of sight.
Our eyesight primarily comprises two distinct functions: central and peripheral vision. Central vision, which relies on the macula's high concentration of cones, enables us to focus on tasks like reading, driving, and recognizing colors and shapes.
Conversely, peripheral vision, which excels in low light conditions due to a higher density of rods, processes spatial information and is essential for our fight or flight response. Though not actively employed like central vision, peripheral vision enhances spatial awareness and body mechanics in various activities. It plays a crucial role in scene gist recognition, helping us access long-term memory and guiding our actions.
 What is retinitis pigmentosa?
What is retinitis pigmentosa?
Retinitis pigmentosa, or pigmentary retinitis, is an eye condition that leads to the gradual loss of vision over time. It occurs due to the retina's breakdown and loss of cells. A sight problem happens when the pigment builds up in the retina. It usually occurs when macrophages or retinal pigment epithelial cells move into the retina and multiply. Melanin from these cells causes vision loss.
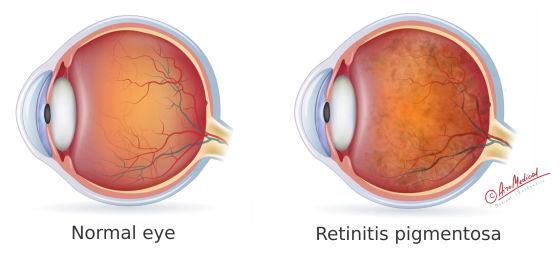 Typically, retinitis pigmentosa initially impacts an individual's rod cells, affecting peripheral (side) vision and enabling sight in low-light or dark environments. People living with retinitis pigmentosa may experience a progressive loss of peripheral vision, eventually leading to tunnel vision.
Typically, retinitis pigmentosa initially impacts an individual's rod cells, affecting peripheral (side) vision and enabling sight in low-light or dark environments. People living with retinitis pigmentosa may experience a progressive loss of peripheral vision, eventually leading to tunnel vision.
Retinitis pigmentosa damages rod cells and can harm other retinal cells over time. It can eventually damage cone cells, which help with central vision, colors, and seeing fine details. So, as the condition gets worse, people may have trouble with both peripheral and central vision, as well as catching colors. That’s the way how does retinitis pigmentosa affect vision.
Retinitis pigmentosa types
There are several types of disorder based on retinitis pigmentosa inheritance:
- Autosomal Dominant Retinitis Pigmentosa (adRP) is inherited when one parent carries a dominant gene mutation. The fact about retinitis pigmentosa is that this form affects individuals with a 50% chance of passing the condition to their children.
- Autosomal Recessive Retinitis Pigmentosa (arRP): Both parents must carry a recessive gene mutation for this form, although they may not have the disease themselves. The affected individual has a 25% chance of inheriting the condition if both parents are carriers.
- X-linked Retinitis Pigmentosa (XLRP) has something to do with the X gene and mainly affects men. Mothers who carry the gene mutation have a 50/50 chance of passing it on to their sons, who will be harmed, and their daughters, who will become carriers.
- Isolated or Simplex Retinitis Pigmentosa occurs without a known family history. It's thought that new genetic changes or a mix of inherited and environmental factors cause it. There are about half of the patients with RP.
These different retinitis pigmentosa types are further divided into subtypes based on the specific gene mutations involved. But the disease's signs and retinitis pigmentosa progression is the same for each type. The main difference is how the disease is passed down.
 What is the cause of retinitis pigmentosa?
What is the cause of retinitis pigmentosa?
Retinitis pigmentosa is caused by genetic mutations affecting the normal functioning of photoreceptor cells in the retina. Depending on the type of disorder, these mutations can be inherited from one or both parents. The genetic mutations result in the breakdown and eventual loss of photoreceptor cells.
As retinitis pigmentosa causes, over 50 genes have been linked with it, with the specific gene mutation determining the exact type and severity of the condition.
Retinitis pigmentosa is primarily caused by these genetic mutations that impact cells in the retina. Inherited from one or both parents, altered genes are passed down through generations. RP, associated with numerous genes, can be inherited in various ways.
Occasionally, retinitis pigmentosa occurs as part of other genetic disorders, such as Usher syndrome, leading to vision and hearing loss.
While less common, RP risk factors can also be certain medications, including antimalarial and other drugs, autoimmune disorders, eye trauma, infection, etc.
How to prevent retinitis pigmentosa?
As you understand, anyone can't prevent retinitis pigmentosa genetics. However, there are some steps you can take to lower the risk of passing it to your children:
- Genetic counseling: If retinitis pigmentosa runs in your family, talk to a genetic counselor before having kids to understand the risks and your options.
- Prenatal testing can detect RP-related mutations during pregnancy. Genetic tests for retinitis pigmentosa can help parents make informed decisions.
- A healthy lifestyle helps maintain eye health and possibly slow retinitis pigmentosa progression. Vitamin A and omega-3 fatty acids might be beneficial.
- Regular eye check-ups can help detect and monitor RP, preserving vision as long as possible.
- Attention to some medications that can affect the retina.
While there's no complete cure for RP, these steps can help manage symptoms and improve quality of life.
 Retinitis pigmentosa symptoms
Retinitis pigmentosa symptoms
RP symptoms can differ for each person but generally start slowly and worsen over time. Since retinitis pigmentosa is a rare and highly varied condition, it can be hard to figure out how often each sign shows up in people with it.
Typical RP signs
What does a person with retinitis pigmentosa see? Here is a summary of common symptoms:
- Night blindness (nyctalopia): Difficulty seeing in low-light conditions or during nighttime; often the first noticeable symptom; almost all patients have it.
- Loss of peripheral vision: Gradual constriction of the visual field leads to "tunnel vision"; affects most patients in the late stage.
- Loss of central vision: As retinitis pigmentosa progresses, central vision may also be affected; it affects many patients, typically in the later stages of the disease.
- Photophobia: Increased sensitivity to light or glare; affects about half of the patients, although the degree of light sensitivity can vary.
- Difficulty adapting to changes in light: Slower adjustment to varying light conditions; a common symptom affecting most retinitis pigmentosa patients.
- Poor color vision: Difficulty distinguishing between colors, particularly in dim lighting conditions; impaired color vision is seen when the disease progresses. Flashes appear in 35% of patients.
- Floaters: Some people with RP may notice floating specks or spots in their vision; the prevalence of floaters in RP patients is not well-established, but it is generally considered a less common symptom.
- Progressive vision loss: Over time, RP may cause blindness in 0,5% of cases; patients with retinitis pigmentosa will experience progressive vision loss, though the rate of progression and severity can vary greatly.
- Headaches appear in 50% of patients.
Even in the same family, these signs of retinitis pigmentosa can be very different in how bad they are and how quickly they get worse. Early detection and treatment are essential for treating the condition and keeping the best quality of life possible.
 Diagnosis of retinitis pigmentosa
Diagnosis of retinitis pigmentosa
RP is usually diagnosed through a series of tests and exams. They look at the structure and function of the retina and medical and family history. Some of them are:
Diagnostic tests
- Family history can help find patterns of inheritance and support a diagnosis of RP if other family members have had similar symptoms or have been diagnosed with the condition.
- Comprehensive eye exam: An ophthalmologist will perform a thorough eye examination, checking for any abnormalities in the retina and other structures of the eye.
- Visual acuity test measures the sharpness of your central vision and can help identify vision problems.
- Visual field test, also known as perimetry. It measures the peripheral (side) vision and is widely used to detect the constriction of the visual field, a common symptom of RP.
- Fundus examination: The doctor will use an ophthalmoscope to examine the back of the eye, including the retina, optic nerve, and blood vessels. In RP patients, the retina may show characteristic changes, such as pigment clumping, "bone-spicule" patterns, or attenuation of blood vessels.
- Full-field electroretinogram (ERG) measures the retina's electrical activity in response to light stimuli. In RP patients, the ERG typically shows a reduced or absent response, indicating the impaired function of the photoreceptor cells (rods and cones). Due to the new research on retinitis pigmentosa, ERG is the gold-standard method for detecting it. ERG can find out if photoreceptors aren't working even if there aren't many changes on a clinical test or with imaging.
- Optical coherence tomography (OCT) is a non-invasive imaging retinitis pigmentosa test that provides detailed, cross-sectional retina images, allowing the doctor to assess its structure and detect abnormalities. OCT also helps to monitor disorder progression.
- Genetic testing: Since RP is a genetic disorder, genetic testing can help identify the specific gene mutation causing the disease in a particular individual. The most common mutation is in the ABCA4 gene (found in 20.8% of patients).
This information can help confirm the diagnosis, provide genetic counseling, and guide treatment decisions.
Depending on the specific case and the patient's symptoms, the diagnostic process may involve additional tests and help to choose how retinitis pigmentosa is treated.
Retinitis pigmentosa stages
Retinitis pigmentosa is a group of eye diseases that cause vision loss over time. It's different for everyone, but we can generally describe three stages:
- Early stage: People have trouble seeing at night and may start losing side vision. They might also find it hard to adjust to different levels of light.
- Middle stage: Side vision loss worsens, leading to "tunnel vision." People may also become more sensitive to light and have trouble seeing colors, especially in dim light.
- Late stage: People lose central vision, which makes it hard to read, drive, or recognize faces. The vision loss may worsen, and some people become legally or entirely blind.
How fast retinitis pigmentosa progress and the severity of vision loss can vary greatly. Early diagnosis and help from eye doctors can improve the quality of life for those with RP.
What countries are the best to treat retinitis pigmentosa?
 Treatments for retinitis pigmentosa
Treatments for retinitis pigmentosa
Concerning the question of whether retinitis pigmentosa be cured, the answer at this level of medical science is no radical treatment. There is no retinitis pigmentosa surgery as well. At the same time, symptomatic treatment available now can help the patient:
Conventional treatment options
- Go for regular eye checkups. The choice of glasses will help you see better.
- Taking supplements with vitamin A, fish oil, or lutein is traditionally used to keep the eyes healthy. However, no differences are found in the studies between taking them to delay the disease progression.
- Use programmable lighting. Light bulbs or fixtures that can be dimmed create an inviting atmosphere at home and work.
- Using a magnifying glass can help you read small writing.
- Move the furniture around. The best way to set up a table at home and work are to create clean, open places and make it much less likely that you will run into something and get hurt.
Despite no cure for retinitis pigmentosa, researchers continue to explore potential treatments and therapies to slow down or halt the progression of the disease and improve the quality of life.
Alternative treatments for retinitis pigmentosa
They include traditional and complementary therapies that may not cure RP but can help improve well-being and quality of life. These treatments include:
- Acupuncture for retinitis pigmentosa: An old practice using thin needles on the body to balance energy and promote healing. Some RP patients think it can help their vision, but limited scientific evidence exists.
- Ayurvedic medicine: A healing system from India focusing on balancing body, mind, and spirit. Practitioners suggest herbs, diet changes, and lifestyle adjustments to help RP patients, but the effectiveness is not well-researched.
- Homeopathy: A treatment using highly diluted natural substances to encourage the body's healing. Homeopathic doctors offer remedies for RP symptoms, but little scientific evidence supports homeopathy's effectiveness in treating RP.
Remember, these alternative treatments' effectiveness must be well-established, and scientific evidence is limited.
Retinitis pigmentosa treatment centers
 New treatments for retinitis pigmentosa
New treatments for retinitis pigmentosa
Over the years, researchers have been exploring different avenues to develop the best treatment for retinitis pigmentosa. Some of the most promising ones are:
Latest surgical options
Retinal implants and prosthetic devices
Argus II Retinal Prosthesis System, also known as the bionic eye, which have been created to help improve vision in people with severe vision loss from RP. These devices change visual information into electrical signals that the remaining retinal cells can understand. In a study with 30 participants, retinitis pigmentosa treatment success of this method was almost 90% of the people who used the device experienced an improved vision, and 80% saw an increased quality of life.
Transplantation
Concerning the eye transplant for retinitis pigmentosa. Like a fiber optic cable, the optic nerve comprises over one million tiny nerve strands. When these nerve fibers are cut, they can't be restored. That’s why you can't replace a whole eye. However, the retina transplant is real. The latest treatment for retinitis pigmentosa is to replace damaged eye cells with healthy ones to restore vision. Two main approaches exist: replacing the entire retina from a donor’s eye and only specific retinal cell transplantation. Both methods are still in the early research stages. Some challenges include survival and integration of transplanted cells, immune rejection, and refining surgical techniques.
Non-surgical solutions
Microcurrent stimulation for retinitis pigmentosa
It brings together the eye and brain science fields. It uses mild electric pulses to stimulate damaged cells in the retina, helping them better send signals to the brain. This electrical stimulation boosts the activity of the whole visual system and helps it recover function. Restorative therapy is a non-surgical approach using electrical stimulation on different cells in the retina (like cones, rods, and ganglion cells). The treatment doesn't replace damaged cells but helps the remaining cells work better.
The stem cell for retinitis pigmentosa
The therapy helps treat it by injecting special retinal progenitor cells into the eye. These cells come from donors or the patient's body and can become retinal cells. They help keep the patient's eye cells healthy and stop them from worsening, saving their vision. Scientists are continuing stem cell research for retinitis pigmentosa with the potential to replace or repair damaged retinal cells in RP patients. While this area of research is still in its early stages, it holds promise for the future treatment of RP.
Genetic treatment for RP
Gene therapy for retinitis pigmentosa
It uses a harmless virus to deliver a healthy copy of the affected gene to the eye's cells. It helps them to work correctly, prevents further vision loss, and improves the prognosis of retinitis pigmentosa. The FDA-approved gene therapy, Luxturna, has successfully improved vision for patients with a specific RP-related gene mutation. Among the retinitis pigmentosa drugs, Luxturna showed up a 93% success rate in Phase III studies with 29 people.
CRISPR-based technique
Researchers have successfully used a new technique called PESpRY to restore vision in mice with RP. The study, published in the Journal of Experimental Medicine, shows that the PESpRY system can correct various genetic mutations, demonstrating its potential for treating inherited eye diseases.
The researchers targeted a mutation in the PDE6β gene in mice with retinitis pigmentosa. Due to the recent advances and breakthroughs in retinitis pigmentosa, using the PESpRY system corrected the mutation, preventing the death of light-sensitive cells in the eye and restoring the mice's vision. Although more work is needed to ensure the safety and effectiveness of this technique in humans, the study offers promising evidence to treat retinal diseases.
As research progresses, we can anticipate even more promising treatment options that will significantly influence the lives of RP patients.
Retinitis pigmentosa specialists
 Retinitis pigmentosa statistics and prognosis
Retinitis pigmentosa statistics and prognosis
Retinitis pigmentosa is the leading cause of retinal degeneration, resulting in blindness. This disease progresses over many years, leading to disability and various limitations. People with retinitis pigmentosa often face significant challenges in their quality of life.
RP statistics
Between 2012 and 2020, Retina Australia conducted a worldwide study of eye patients and some retinitis pigmentosa statistics. They found that 1% of patients were diagnosed with RP. Of these, 34.3% experienced mild central vision loss or none at all, 44.4% showed signs of retinal damage, and 21.3% became legally blind.
AiroMedical's analysis reveals that most people with retinitis pigmentosa experience a significant decline in visual acuity in their 30s. As a result, over half of these patients could benefit from new treatments. Prompt access to specialists is essential for planning and selecting the appropriate treatment options.
References:
- Sanie-Jahromi, F., Azizi, A., Shariat, S., & Joharicorresponding, M. (2021). Effect of Electrical Stimulation on Ocular Cells: A Means for Improving Ocular Tissue Engineering and Treatments of Eye Diseases. Biomed Res Int, 2021, 6548554. https://doi.org/10.1155/2021/6548554
- Voisin, A., Pénaguin, A., Gaillard, A., & Leveziel, N. (2023). Stem cell therapy in retinal diseases. Neural Regeneration Research, 18(7), 1478-1485. https://doi.org/10.4103/1673-5374.361537
- Halioua-Haubold, C.-L., Jolly, J. K., Smith, J. A., Pinedo-Villanueva, R., Brindley, D. A., & MacLaren, R. E. (2019). Potential lifetime quality of life benefits of choroideremia gene therapy: projections from a clinically informed decision model. Eye (Lond), 33(8), 1215-1223. https://doi.org/10.1038/s41433-019-0492-1
- O'Neal, T. B., & Luther, E. E. (2023). Retinitis Pigmentosa. In StatPearls [Internet]. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK560738/
- Reference List Citation: Oh, J. K., Nuzbrokh, Y., de Carvalho, J. R. L., Jr, Ryu, J., & Tsang, S. H. (2020). Optical Coherence Tomography in the Evaluation of Retinitis Pigmentosa. Ophthalmic Genet, 41(5), 413-419. https://doi.org/10.1080/13816810.2020.1780619