Retinal Detachment Guide

Less than 1 out of every 10,000 people have a retinal detachment (RD).
Retinal detachment mainly affects people between the age of 60 and 70.
Severe myopia (-6.00 diopters or higher) is associated with a 21-fold greater risk of RD.
The success rate of retinal detachment surgery would be more than 90% if performed during the week.
 Shortly about retina
Shortly about retina
The retina is a thin layer of tissue that lines the back of the eye. Its primary function is to convert light into electrical signals sent to the brain through the optic nerve, allowing us to see.
Anatomy of the retina
The retina contains specialized cells called photoreceptors (rods and cones) responsible for detecting light and color. These cells are supported by other cells, such as bipolar cells and ganglion cells, which help to transmit the signals from the photoreceptors to the optic nerve.
The vitreous body is a clear gel substance that holds the retina to the back of the eye. It stays round inside the eyeballs. It can sometimes shrink or get smaller. It changes the shape of the eyeball and pulls on the retina. When the vitreous pulls on the retina, it pulls away from the eyeball.
The retina is a complex and delicate structure; damage or detachment of the retina can lead to vision loss or blindness.
 What is retinal detachment?
What is retinal detachment?
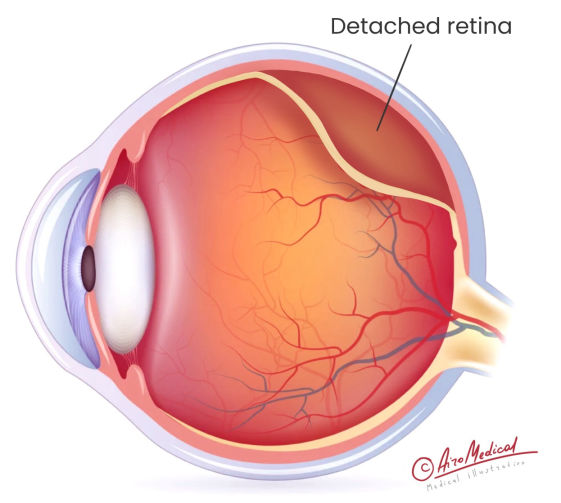 RD is a medical condition when the retina pulls away from the place where it should be. It makes the retinal cells separate from the blood vessels layer, giving the eye oxygen and food. If the retina comes away from the back of the eye, it can't send signals to the brain. It can change your vision or cause you to lose it if you don't treat retinal detachment. The longer the situation goes unchecked, the more the risk of losing sight permanently.
RD is a medical condition when the retina pulls away from the place where it should be. It makes the retinal cells separate from the blood vessels layer, giving the eye oxygen and food. If the retina comes away from the back of the eye, it can't send signals to the brain. It can change your vision or cause you to lose it if you don't treat retinal detachment. The longer the situation goes unchecked, the more the risk of losing sight permanently.
What types of retinal detachment exist?
- Rhegmatogenous retinal detachment is the most common type and happens when a defect appears in the retina. It is called a tear or hole that lets fluid get under the retina and causes it to detach. This situation can occur due to aging, or other eye conditions, such as traumatic retinal detachment.
- Tractional retinal detachment occurs when scar tissue on the retina’s surface pulls it away from the back of the eye. It is often linked to diabetic retinopathy or other eye conditions that cause abnormal blood vessel growth.
- Exudative retinal detachment happens when fluid builds up under the retina and causes it to detach. It is usually started by other underlying medical conditions like inflammation or tumors and is not typically due to a tear or hole in the retina.
 What causes retinal detachment?
What causes retinal detachment?
Retinal detachment can also occur spontaneously without any apparent cause, and it's estimated that it affects about 1 in 10,000 people annually. Additionally, certain activities, such as high-impact sports or activities involving rapid altitude changes–scuba diving or flying, may increase the risk.
Regular check-ups are recommended for everyone, but especially for those of a particular age or with health conditions like diabetes, eye surgery, trauma, etc. People with any of these risk factors should be especially vigilant about getting regular eye exams to detect retinal detachment early.
Common risk factors
Several factors may increase a person's risk of developing RD. These include:
- Age: Retinal detachment is more common in older adults, especially those over 50.
- Eye trauma: A blow to the eye or other injury can cause a tear or hole in the retina and can be the factor that retinal detachment causes.
- Family history: A genetic predisposition may increase risk if a close family member has RD.
- Eye conditions: Certain eye diseases, such as lattice degeneration or posterior vitreous detachment, can cause RD.
- Previous eye surgery: People with cataract surgery or other eye interventions may be at risk for retinal detachment.
- Nearsightedness: People who are nearsighted (myopic) may have a higher chance of getting a retinal tear.
- Certain medical conditions: Diabetic retinal detachment is often a complication because the increased sugar level affects the blood vessels in the eye and can cause retinal defects.
- Extreme sports and activities. They can increase the risk of retinal detachment due to high-impact blows, sudden movements, and changes in pressure. Scuba diving, skydiving, boxing and martial arts, rock climbing, skiing, and snowboarding are some examples of activities that may increase the risk of retinal detachment.
Not everyone with these risk factors will develop this health issue; some may have the condition without any of them. So, any warning signs of retinal detachment we tell below need urgent medical help.
People with underlying eye conditions or a history of retinal detachment may be at higher risk and should take extra precautions or avoid these activities altogether.
How to prevent retinal detachment?
Most RDs occur suddenly, impairing central vision for a few hours or days. And it may not always be real to prevent retinal detachment, but there are steps you can take to lower your risk:
- Get regular eye exams. They can help detect eye changes that may increase your risk. If you are at higher risk, your eye doctor may recommend more frequent exams.
- Protect your eyes: Wear protective eyewear during activities that could cause eye injuries, such as sports or DIY projects.
- Manage chronic conditions: If you have a medical issue affecting your eyes, such as diabetes, ensure you manage it properly to help prevent retinal problems.
- Seek prompt treatment for eye problems: If you experience any sudden problems in your vision, such as flashing lights, floaters, or a shadow in your peripheral vision, seek immediate medical attention. Early treatment can help prevent RD or reduce its severity.
- Know your risk factors: If you have any potential risk factors, be aware of the symptoms of a detached retina and discuss them with your eye doctor.
 What are the symptoms of retinal detachment?
What are the symptoms of retinal detachment?
Recognizing the symptoms of retinal detachment is crucial for timely diagnosis and treatment—most patients with retinal detachment report experiencing some symptoms before being diagnosed. For example, sudden flashes and floaters affect about 66% of people over 70. About 1 of every four patients with retinal detachment reports light flashes of light.
Typical signs of a detached retina
If you experience these symptoms, see a doctor immediately:
- Floaters show up all of a sudden. It is when small spots or particles that look like cobwebs, dots, or lines appear in your field of vision.
- Flashes of light: You may see flashes of light that look like lightning streaks or flashing lights.
- Blurred vision: Your vision may become blurry suddenly or slowly over time. It may be only partially blurry or completely blurry. It is one of the most frequent detached retina symptoms.
- Shadow or curtain over the field of vision: You may see a shadow or something that looks like a curtain over part of your vision.
- Loss of side (peripheral) vision: You may notice your side vision worsening, which can lead to tunnel vision.
Bilateral retinal detachment can cause both eye problems, often leading to complete blindness. So, be attentive to any retinal detachment symptoms that happen quickly and become worsening. They may not be painful. If you have one or several of these, see a doctor urgently.
 How to diagnose retinal detachment?
How to diagnose retinal detachment?
RD is a medical emergency that must be treated immediately. A dilated funduscopic exam is the gold standard for diagnosing retinal detachment.
To determine RD, you need to check your eyes. First, the eye doctor or ophthalmologist looks at the retina after widening the patient's pupil. Eye drops are used to do this. The doctor can examine the fundus a few minutes after putting them in.
Diagnostic methods
For a more exact and thorough checkup, the doctor may suggest the following:
Optical coherence tomography (OCT)
The test helps diagnose and manage retinal detachment. It creates high-resolution images of the retina, allowing ophthalmologists to see the layers of the retina and identify any abnormalities. OCT monitors the treatment progress for RD and assesses the procedure’s success. Optical coherence tomography (OCT) imaging can detect structural changes that may not be clinically evident on fundus examination in patients with RD.
On OCT images, doctors got 97% sensitivity, while on fundus photos, they got only 75%. In another study, the researchers found the changes in the shape of a retinal detachment that can be seen on OCT scans can be used to predict how well the eye will see after surgery.
An ultrasound exam of the eyes
It is another imaging modality that can be used for RD diagnosis and management; it is beneficial when the view of the retina is obscured, such as when there is blood or other opacities in the eye. The sound waves bounce off the tissues inside the eye, create an image of the retina on a screen, and help ophthalmologists identify abnormalities. The ultrasound test had 100% sensitivity. It is a good and accurate way to find retinal tears. Repeated ultrasound exams can help to determine whether the detachment improves, worsens, or remains stable.
It is essential to know that retinal disease mainly does not improve without treatment. So, getting a diagnosis and continuing treatment is vital to keep your vision or get it back. Most treatments work well if they are done quickly. But vision may take a while to get better, and some damage may be permanent in severe cases.
Some words about the severity of the disease
RD can range from mild to severe, depending on the extent of the detachment and the underlying cause. The severity is determined by several factors, including:
- Type: There are different RD types, and each has nuances in outcomes.
- Size can vary from a small area to the total retinal detachment that needs immediate treatment.
- The location can also impact the severity of the condition. Detachments in the macula, the central part of the retina responsible for sharp, detailed vision, are more severe than issues in the periphery.
- Speed of onset: RD can occur suddenly or gradually. A sudden one is usually more severe and requires prompt treatment. Untreated chronic retinal detachment also leads to vision loss.
- Underlying causes can also impact its severity. For example, a detachment caused by trauma or inflammation may be more severe than one caused by aging.
The severity of the condition can also affect the treatment options and the likelihood of successful reattachment. It's essential to seek medical attention as soon as possible if you experience any RD symptoms to prevent permanent vision loss.
Second medical opinion
Sometimes, a second opinion may be necessary, especially if not all doctors are ready to perform a secondary operation. It is where AiroMedical comes in, offering a remote consultation service to help patients get a second opinion from an experienced retinal specialist. This service can benefit those who live in remote areas, have difficulty traveling to a doctor or want to explore all their options before surgery.
Where to go if somebody has retinal detachment?
 Treatment of detached retina
Treatment of detached retina
Almost all people with retinal problems need surgery to restore their lives. In highly unusual cases, a retinal detachment may heal without the patient realizing it happened. So, retinal detachment treatment options include various surgical methods, preferably less invasive.
Types of retinal surgeries
Surgery usually doesn't require a hospital stay, so that the person can go home on the same day. Without the surgery, the retina might lose its ability to work, making it impossible to see. The way how to treat retinal detachment depends on what causes it.
Scleral buckle
The doctor puts a small, flexible bandage on the sclera, which is the white part of the eye. The tape then puts light pressure on the sides of the eye, which helps the retina stick back together. After the operation, the patch will always be on the look. The initial anatomical success rate reached 92.7%, finally in all 100%.
Pneumatic retinopexy
The procedure closes a small tear that is easy to fix. A tiny bubble of gas is put into the vitreous by the ophthalmologist. The bubble's pressure on the top part of the retina completes the gap. For the bow to stay in the right place, you sometimes must keep your head in a particular position for several days. Concerning the effect, researchers claim that pneumatic retinopexy to filtered air works in 85.7%–86.7% of cases.
A vitrectomy
It is done outpatient for large tears. During the surgery, a small cut is made in the sclera, the vitreous body is surgically removed, and a bubble of air, gas, or oil is put in the eye to help the retina move back into place. The success rate of the first reattachment procedure was 93.5%.
Most of the time, the procedures are painless but may cause discomfort. The person can leave the hospital on the same day. You must wear an eye patch for several days and avoid strenuous activities.
Complications of retinal detachment surgery
If the detachment isn't taken care of quickly, it can cause the eye to lose sight completely. Some of the complications can occur after eye surgery:
- Proliferative vitreoretinopathy (PVR) can occur after RD surgery. The growth of scar tissue on the retina or inside the eye can cause a recurring detached retina.
- Cataracts are a common complication of surgical procedures for retinal detachment. They occur when the eye’s natural lens becomes cloudy, which can cause blurry vision. As estimated, 1 in every four patients had it.
- Glaucoma is a group of eye conditions that can damage the optic nerve and lead to vision loss. Detached retinal surgery can increase the risk of its development.
RD surgery has a high success rate. Still, failed retinal detachment surgery treatment occurs. It may be due to complications such as infection or scar tissue formation, new tears or holes in the retina, or pre-existing eye conditions. Additional surgery may be necessary with the success rate depending on the cause of failure and overall eye health. The patient may need a vitrectomy to remove scar tissue and reattach the retina.
Hospitals where are ready to help
 New treatment for retinal detachment
New treatment for retinal detachment
As technology and medical knowledge advance, new approaches are being developed to treat retinal detachment. One such company working to investigate new solutions is AiroMedical, which uses AI to aid in the remote diagnosis and finding of the most effective and non-invasive treatment of eye diseases.
According to a study, retinal detachments can be fixed with the latest surgery techniques with more than a 90% success rate after the first procedure.
Advanced treatments
The procedure aims to connect the retina to the back of the eye and close the breaks or gaps that induced the detachment. Doctors can also use the following methods:
Photocoagulation, or laser treatment for retinal detachment
It is the most advanced surgical method. This surgery is used when there is a problem with the eye’s vitreous body. The laser burns through the tear, leaving scars. This granulation tissue helps seal the tear or connect a piece of the retina that has come loose to the tissue underneath. With retinal tears, the procedure keeps fluid from getting under the retina, which could cause the retina to pull away from the back of the eye.
Due to the study, localized photocoagulation was successful in 96.4% of cases, while 360-degree laser treatment was effective in 95.8% of cases.
Cryopexy
The procedure uses extreme cold to create a scar on the retina, which helps to hold it in place in case of small tears or holes. It is typically done outpatient and takes about 20-30 minutes. While it is generally considered safe and effective, additional methods may be necessary. With retinal cryopexy, 94.9% of cases were fixed after just one surgery.
The bionic retinal implant
It is either the end of eye care technology or a big step forward. During the process, a 2 mm microchip is surgical intervention implanted in the center of the retina, and a pair of special video glasses are attached to a computer on the belt. The chip sends the data the glasses record about what you see to a computer. It then uses AI algorithms to process the data and tell the glasses to focus on the main subject. The glasses send this information to a chip, turning it into an electric signal. The eye and optical cells send this signal to the brain, where it is read as real vision.
Results are promising - 80% of the patients' vision has improved, and about 40%can see much better.
What are alternative treatments for a detached retina?
Some ongoing research exists on using stem cells for a detached retina. Stem cells are unique cells that can develop into various kinds of cells, including those found in the retina.
One approach is using mesenchymal stem cells (MSCs), which have shown promise in preclinical studies for repairing damaged retinal tissue. In animal models, MSCs have been shown to improve retinal function and promote the survival of retinal cells after a detachment. Due to another study, at the 12-month follow-up, 90.6% of patients whose stem cells were given intravenously improved their vision.
However, more studies are needed to understand how safe and effective the new treatment for a detached retina is. Stem cell therapy is not considered a standard treatment option and is not widely available outside clinical trials.
Meet our best retinal detachment specialists
 Stats and prognosis of retinal detachment
Stats and prognosis of retinal detachment
Statistics play a crucial role in evaluating the success rate of medical procedures such as retinal detachment surgery. In this context, statistics help to determine the probability of the operation's success and the likelihood of vision recovery.
By offering access to qualified ophthalmologists and technologies, AiroMedical ensures patients receive prompt and efficient care. By utilizing statistical data and the expertise of medical professionals, AiroMedical is committed to delivering the best possible outcomes for patients undergoing retinal detachment surgery.
The success rate for retinal detachment surgery
In most highly specialized eye centers AiroMedical offers, about 90% of retinal detachments can be fixed with just one surgery. In other cases, the retina detaches again, and a second surgery is needed. The success rate, in the end, is over 95%.
The operation's success and the detachment's length, size, and location determine vision recovery. The macula, which governs center vision, may be loose. The patient may never see well again after surgery.
The prognosis for vision improvement
How well RD will heal depends on the severity of the tear and the patient's overall health. Due to the study, the macula's attachment exacerbates a hole or tear in the retina, known as rhegmatogenous retinal detachment. 83% of patients report improved eyesight when the macula is undamaged. Yet, the outlook for vision recovery is bleak if the macula is detached.
After surgery, 37% of patients with macula-off detachment regained good vision within the first week, according to research. Some patients require surgical intervention within the first week. Submacular fluid, however, may worsen the prognosis for visual recovery. A patient's phakic state does not affect the visual prognosis.
The visual outlook for patients with tractional retinal and exudative RD types varies according to the condition's causes and other vision-impairing disorders.
How to choose the proper treatment? A professional ophthalmologist can advise you after thorough eye and retinal tear examinations. Therapies typically work together: scleral filling and vitrectomy can be done combined.
Most importantly, a detached retina does not recover on its own. So, to preserve vision, the patient must see a doctor immediately. AiroMedical is here to find your best eye doctor for a detached retina. Our form is available. Just fill it out; we can offer a solution without delay.
References:
- Botwin A, Engel A, Wasyliw C. The use of ocular ultrasound to diagnose retinal detachment: a case demonstrating the sonographic findings. Case Reports in Emergency Radiology. 2018;25(4):445-447. doi: 10.1007/s10140-018-1585-z. PubMed PMID: 29404803.
- Cole CJ, Charteris DG. Cataract extraction after retinal detachment repair by vitrectomy: visual outcome and complications. Eye. 2009;23:1377-1381.
- Blair K, Czyz CN. Retinal Detachment. [Updated 2022 Oct 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537332/
- Jalali S. Retinal detachment. Community Eye Health. 2003;16(46):25-26. PMID: 17491854; PMCID: PMC1705859.
- Lin Y, Ren X, Chen Y, Chen D. Interaction between mesenchymal stem cells and retinal degenerative microenvironment. Front Neurosci. 2020;14:617377. doi: 10.3389/fnins.2020.617377. PMID: 33551729; PMCID: PMC7859517.
- Auger, G., & Winder, S. (2011). Spectral Domain OCT: An Aid to Diagnosis and Surgical Planning of Retinal Detachments. Journal of ophthalmology, 2011, 725362. doi: 10.1155/2011/725362. PMID: 22254129. PMCID: PMC3255307.