Alzheimer's Disease (AD) Guide

Alzheimer's causes about 60–70% of all dementia cases worldwide.
Age is the biggest risk factor for Alzheimer's: more than 30% of 85+ have it.
One-third of seniors die because of Alzheimer's or another form of dementia.
After a diagnosis of Alzheimer's, life expectancy is 4–8 years, but it could be as long as 20 years.
 Some info about brain
Some info about brain
Several brain structures contribute to our identity, thoughts, emotions, and behavior:
- Prefrontal cortex: Responsible for decision-making, planning, and social behavior, it shapes our personality.
- Hippocampus: Essential for memory formation, it helps remember experiences that form our history.
- Amygdala: Involved in processing emotions and emotional memory, it influences our behavior and reactions.
- Cerebral cortex: Responsible for higher-order functions like thought and perception, it contributes to our learning abilities.
- Thalamus: Regulates consciousness, sleep, and alertness, affecting our daily experiences.
- Basal ganglia Influence movement, reward, and habit formation shaping our routines and motor skills.
These structures work together, shaping our thoughts, emotions, and actions that make us who we are.
 So, what is Alzheimer's disease?
So, what is Alzheimer's disease?
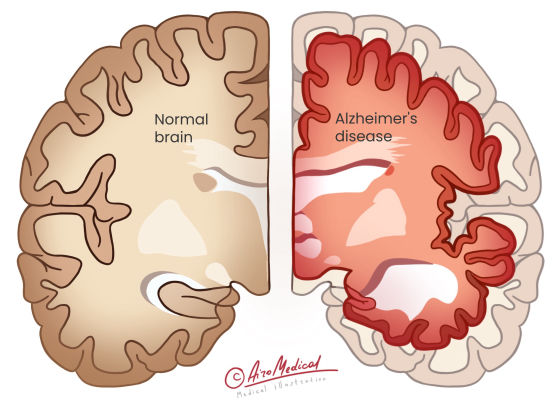
AD mainly affects the hippocampus and cerebral cortex, essential brain parts for memory, thinking, and higher-level functions. Changes to the prefrontal cortex can impact how people make decisions. Alzheimer's disease alters a person's identity and behavior, making it harder for the brain structures we told earlier to work together. It is named after Alois Alzheimer, the physician who first described it.
Development of the disease
 Two main hallmarks characterize the development of Alzheimer's:
Two main hallmarks characterize the development of Alzheimer's:
- Amyloid plaques are unusual clumps of a protein fragment called beta-amyloid that build up between brain cells. The plaques disrupt communication between neurons or nerve cells, resulting in their death.
- Neurofibrillary tangles are strands of tau protein found inside brain cells. It changes and forms tangle that slow the transport of nutrients within brain cells, leading to their death.
Alzheimer's disease is irreversible and worsens over time, ruining memory and thinking skills and, finally, the possibility of doing even the most manageable everyday tasks.
Concerning what type of doctor treats Alzheimer’s will be a team of professionals, including a primary care physician, a neurologist, and a geriatric psychiatrist.
Types of Alzheimer's disease
Based on what age Alzheimer's starts, there are two main types of the disease:
Late-onset Alzheimer's is the most common form, usually affecting people aged 65+. The cause of Alzheimer's is unclear. But, it might involve a mix of genes, environment, and lifestyle. APOE ε4 gene is a significant risk factor.
Early-onset Alzheimer's is a rare form that affects people younger than 65, with symptoms appearing in their 40s or 50s. It has two subtypes:
- Familial Alzheimer's genetic is an inherited type caused by specific gene mutations (APP, PSEN1, or PSEN2).
- Non-familial Alzheimer's has no known gene mutations or clear inheritance patterns. The cause might involve a mix of genes, environment, and lifestyle.
Research on Alzheimer’s disease is ongoing to determine if there are more subtypes based on how the disease progresses and worsens in different people.
 What causes Alzheimer’s?
What causes Alzheimer’s?
Having one or more risk factors doesn't necessarily mean a person will develop the disorder. However, understanding and managing these factors may help delay the onset.
Who is at risk for AD?
Risk factors for Alzheimer's disease include:
- Age: The risk of developing Alzheimer's increases with age. Most people diagnosed with the disease are 65 years old or older.
- Family history: Individuals with a parent or sibling with Alzheimer's are at a higher risk of developing the disease.
- Genetics: Certain genes, such as the APOE-e4 gene, have been related to a more increased risk of AD.
- Lifestyle factors: A bad diet, not getting enough exercise, smoking, and drinking too much alcohol can all increase the risk of Alzheimer's.
- Head injuries: A history of head trauma or brain injuries may increase the risk later.
- Cardiovascular disorders: High blood pressure, heart diseases, stroke, diabetes, and high cholesterol raise Alzheimer's risk.
- Education level: Fewer years of schooling may be associated with a higher risk of Alzheimer's.
Alzheimer's prevention
To help prevent Alzheimer's disease, consider these lifestyle choices:
- Exercise regularly: Engage in physical activity for at least 150 minutes per week, combining aerobic exercise and strength training.
- Eat a healthy diet: Focus on a balanced diet. Include fruits, vegetables, whole grains, lean proteins, and healthy fats, such as the Mediterranean or DASH diet.
- Maintain a healthy body weight with a balanced diet and regular exercise.
- Get quality sleep: Aim for 7-9 hours per night, and treat sleep disorders if necessary.
- Manage stress: Practice stress-reduction techniques such as meditation, yoga, or deep breathing.
- Stay mentally active: Engage in mind-stimulating activities to keep the brain challenged.
- Be socially active: Maintain solid relationships and participate in social activities to support mental and emotional health.
- Control cardiovascular risk factors: Maintain normal blood pressure, blood sugar, and cholesterol.
- Quit smoking to reduce your risk.
- Limit alcohol intake, sticking to the recommended guidelines.
Remember that while these strategies may help reduce the risk of Alzheimer's, they cannot guarantee complete prevention.
 Alzheimer’s disease symptoms
Alzheimer’s disease symptoms
We use only evidence-based data. However, concerning Alzheimer's disease, it's difficult to provide precise numbers regarding the symptoms, as they can vary.
Typical signs
Here are some general observations:
- Memory problems are the most common symptom, affecting nearly all Alzheimer's patients as the disease progresses.
- Language difficulties finding the right words or understanding conversations occur in approximately 80% of patients.
- Difficulties with problem-solving and complex tasks have about 60% of Alzheimer's patients.
- Spatial and visual problems such as misjudging distances and having trouble reading or color vision occur in around 40%-50% of patients.
- Apathy, social withdrawal, and loss of interest in previously enjoyed activities are common, affecting up to 88% of individuals with Alzheimer's.
- Mood and personality changes, including depression, anxiety, irritability, and paranoia, can be seen in up to 50% of Alzheimer's patients.
- Sleep problems have 25-40% of mild-to-moderate Alzheimer's patients. These are napping during the day and trouble sleeping at night.
- Depression faced nearly half of Alzheimer's patients.
Sadly, around 60% of Alzheimer’s disease patients wander and get lost frequently.
What are Alzheimer’s early signs?
Answering the question of how Alzheimer’s starts, the early signs include:
- Memory loss disrupts daily life, such as forgetting recently learned information or important dates.
- Challenges in planning or solving problems, like following a recipe or managing bills.
- Difficulty completing familiar tasks, such as driving to known locations or organizing a grocery list.
- Confusion with time or place, losing track of dates, seasons, or locations.
- Losing understanding of visual images and spatial relationships leads to balance or reading issues.
- Problems with speaking or writing, needing help to follow conversations or find the right words.
- Misplacing things, losing the ability to retrace steps, with items placed in unusual locations.
- Decreased or poor judgment, such as mishandling money or neglecting personal hygiene.
- Withdrawal from work or social activities, losing interest in hobbies, or needing help to engage in conversations.
- Mood changes, becoming confused, suspicious, depressed, or anxious.
How fast Alzheimer’s progress depends on a variety of factors. Anyway, early diagnosis and intervention can help manage the disease better.
 How is Alzheimer’s diagnosed?
How is Alzheimer’s diagnosed?
There still isn't a definitive test for Alzheimer's disease. Diagnosis involves identifying particular symptoms and excluding other causes, involving multiple steps:
Diagnostic steps
- Thorough history taking, including medical history, family history, and any changes in memory, behavior, or personality.
- Mental status checks: Assessing cognitive abilities, such as memory, attention, language, and problem-solving skills, through mini-mental state examination (MMSE).
- Physical examination: A general health check to identify or rule out other possible causes of dementia-like symptoms.
- Neurological examinations: Evaluating reflexes, coordination, balance, and other sign of neurological conditions.
- Blood tests check for vitamin deficiencies, thyroid problems, or other conditions leading to cognitive decline.
- Genetic testing: Alzheimer’s gene test that helps identify an individual's risk includes specific APOE and presenilin genes.
These assessments help doctors determine the presence of Alzheimer's disease and rule out other potential causes for the symptoms.
Imaging tests
Brain imaging studies play a crucial role in diagnosis, helping to identify changes in the brain. Some standard imaging techniques include:
- Magnetic Resonance Imaging (MRI): MRI scans provide detailed images of the brain, helping to detect shrinkage in areas like the hippocampus associated with Alzheimer's disease. MRIs also help to identify tumors or strokes.
- Computed Tomography (CT) scans: CT scans offer a less detailed view of the brain than MRI scans. However, they still help identify significant brain atrophy and discover other conditions causing dementia-like symptoms.
- Positron Emission Tomography (PET) scans can assess brain metabolism and help identify amyloid plaques, and signs of AD. PET brain scans for Alzheimer’s use a special tracer that binds to amyloid plaques, making them visible on the scan.
- Tau PET scans also use a tracer that binds to tau protein tangles, another AD hallmark. This advanced technology can be done in Alzheimer’s disease research centers.
These techniques provide proven evidence of the changes connected with Alzheimer's disease and can aid in diagnosing.
Stages of Alzheimer
AD progresses through various stages:
- Preclinical: No noticeable symptoms, but brain changes are occurring.
- Mild cognitive impairment (MCI): Subtle cognitive changes without significantly impacting daily life.
- Mild Alzheimer's (early-stage): More pronounced memory loss, difficulty planning and organizing, and mood changes.
- Moderate Alzheimer's (middle-stage): Severe memory loss, challenges in recognizing familiar faces, and difficulty managing personal hygiene and routine tasks.
- The late stage of Alzheimer's (severe/advanced) involves severe memory loss, loss of communication, physical decline, and increased susceptibility to infections—the focus of Alzheimer's care shifts to comfort and quality of life.
How to differentiate Alzheimer's & dementia
Alzheimer's disease and dementia are related but different. Dementia is a decline in cognitive abilities severe enough to interfere with daily functioning. Alzheimer's is dementia, the most common type, with about 60-70% of cases.
The difference between dementia and Alzheimer's is in the:
- Symptoms: While memory loss is common in Alzheimer's and other dementias, other cognitive and behavioral symptoms may vary depending on the type of dementia.
- Progression: Alzheimer's typically follows a gradual progression, while other dementias may have a more abrupt onset or rapid decline.
- Brain imaging: MRI or CT scans can reveal specific brain atrophy.
- Specific tests: Blood tests or lumbar punctures can help identify biomarkers associated with Alzheimer's or other forms of dementia.
In short, to find the difference between Alzheimer's disease and dementia, we need to involve assessing symptoms, progression, and diagnostic tests.
Where to find a treatment
 Treatments for Alzheimer’s disease
Treatments for Alzheimer’s disease
The question of how to treat Alzheimer's still not has a definite answer. Conservative therapy for Alzheimer's disease primarily aims to manage symptoms and improve the quality of life. If you want to know if Alzheimer's is curable, it is sad, but no one can recover.
Common treatment options
At the same time, some remedies can help slow cognitive decline and manage behavioral symptoms:
- Cholinesterase inhibitors increase acetylcholine levels, a neurotransmitter that plays a crucial role in learning and memory. Cholinesterase inhibitors can help to slow the progression of Alzheimer's in some patients.
- Memantine (Namenda) regulates the activity of neurotransmitters involved in learning and memory. It can help with symptoms in moderate to severe Alzheimer's cases.
- Antidepressants can be prescribed to address depression or anxiety, which is common in people with Alzheimer's.
- Antipsychotics are used when patients with Alzheimer's have agitation, aggression, or hallucinations.
- Sleep aids: Assleep disturbances are common in Alzheimer's. Doctors may prescribe sleep aids or recommend over-the-counter options.
- Memory improvement medications should be tailored to each patient's symptoms.
Non-drug treatments
Besides medication for Alzheimer’s, non-drug approaches exist. Among them, mental and physical exercise and a nutritious diet can also enhance well-being and daily functioning.
Specialized rehabilitation programs focus on particular Alzheimer's symptoms or stages. Some programs focus on improving memory, making it easier for people to do everyday tasks independently, and controlling behavioral symptoms. Doctors, nurses, and occupational, physical, and speech therapists are part of a team that works on these programs.
Top Alzheimer’s hospitals
 New treatment for Alzheimer’s
New treatment for Alzheimer’s
The fight against Alzheimer's has been slow and sometimes disappointing progress over the past ten years. Scientists are still finding a cure for Alzheimer's disease to determine how the brain changes and worsens. Researchers are also working diligently to discover how to treat it with a drug.
New Alzheimer's medications
Aduhelm
The drug, also known by its generic name aducanumab, is a targeted drug recently approved by the US Food and Drug Administration (FDA) for treating early Alzheimer's disease. This new Alzheimer’s medication is the first therapy approved by the FDA to target plaque-forming beta-amyloid. Plaques may kill brain cells and tissue in memory, thinking, learning, and behavior. Aducanumab reduces brain beta-amyloid production. Eliminating it may improve other brain functions.
Leqembi
It is Alzheimer’s new drug approved by FDA in 2023 and is another drug for early-stage AD. In a large clinical trial, patients who took Leqembi had a 70% decrease in A-plaques after 79 weeks of treatment, as measured by a PET scan. Patients who did not take Leqembi had a slight increase in A-plaques.
However, the drug's efficacy and safety are still being studied, and there are concerns about its potential side effects. At the same time, it represents a new approach to treating Alzheimer's disease.
Alternative treatments for Alzheimer’s
Adopting a healthy lifestyle and lowering the possibility of cognitive decline and dementia is an alternative approach. It often describes different medicines, supplements, and medical nutrition. But the mission statement about their safety and effectiveness is mainly based on what other people have said, on tradition, then on scientific research.
Vaccine for Alzheimer’s is another approach to treatment. Researchers claim it can reduce brain inflammation in people with early Alzheimer's disease. The trial should be over by the fall of 2023.
How can stem cells help Alzheimer’s disease?
Stem cells may treat Alzheimer's as they become nerve cells and may replace damaged brain nerve cells, according to research. It may assist Alzheimer's patients in regaining brain function.
Some early investigations on Alzheimer's disease stem cell therapy have shown promise. In a small clinical experiment, neural stem cell patients performed better at everyday tasks and cognitive function than those who received a placebo.
Before stem cell treatment can cure Alzheimer's, many issues must be resolved. They include finding safe and effective techniques to deliver stem cells to the brain.
Stem cell treatment option for Alzheimer's gives us hope. However, its pros and cons need further study.
Meet the best doctors for Alzheimer’s disease
 Statistics on Alzheimer’s
Statistics on Alzheimer’s
A person somewhere in the world gets Alzheimer's every three seconds.
The Alzheimer's Association says there are 24 million people with Alzheimer's worldwide, which is expected to double every 20 years till at least 2040. Alzheimer's disease is not completely understood to be what causes it, but some things are thought to increase the risk of getting it.
Stats and figures
Alzheimer's disease is most likely to happen because of getting older. Alzheimer's disease affects many more people as they age 5.3% of people 65 to 74 have it, 13.8% of people 75 to 84, and 34.6% of people 85 and older.
Alzheimer's disease is the sixth leading cause of death in the United States, and deaths have increased by 145% since 2000. In 2021, the estimated cost of caring for individuals with Alzheimer's and other dementias in the United States was $355 billion. This cost is projected to rise to $1.1 trillion by 2050.
Alzheimer's disease affects the individual with the disease and significantly impacts caregivers. In 2020, more than 11 million Americans provided unpaid care for someone with Alzheimer's or another form of dementia, with caregivers providing an estimated 15.3 billion hours of care valued at $257 billion.
Alzheimer's prognosis
Alzheimer's disease affects people differently at different stages. Those with a moderate set may have trouble speaking and solving problems. The disease may worsen memory loss, confusion, and personality and behavior abnormalities. Later in the condition, patients may be bedridden and need 24-hour care.
The type of AD affects prognosis. Alzheimer’s statistics show that early-onset Alzheimer's disease begins before 65 and may cause faster cognitive decline.
There is no cure for Alzheimer's disease, although some therapies can improve symptoms and quality of life. New drugs for Alzheimer’s and cognitive and behavioral therapies can temporarily improve memory and brain function. Early detection and treatment are vital to slowing the progression.
How to decide which treatment is best? After a thorough neurological exam, a trained neurologist can give you advice. Most therapies work well together and can be done at the same time.
Most important, Alzheimer's gets worse faster if it isn't treated. So, see a doctor immediately to keep as much of the patient's personality and independence as possible. We're here to help you find the top Alzheimer’s doctors. Just fill it out, and we can help you right away.
References:
- Jahn, H. (2013). Memory loss in Alzheimer's disease. Dialogues in Clinical Neuroscience, 15(4), 445-454. doi:10.31887/DCNS.2013.15.4/hjahn. PMCID: PMC3898682. PMID: 24459411.
- Moran, M., Lynch, C. A., Walsh, C., Coen, R., Coakley, D., & Lawlor, B. A. (2005). Sleep disturbance in mild to moderate Alzheimer's disease. Sleep Medicine, 6(4), 347-352. doi:10.1016/j.sleep.2004.12.005. PMID: 15978517.
- Armstrong, R. A. (2009). Alzheimer's Disease and the Eye. Journal of Optometry, 2(3), 103-111. doi:10.3921/joptom.2009.103. PMCID: PMC3972797.
- Nobis, L., & Husain, M. (2018). Apathy in Alzheimer's disease. Current Opinion in Behavioral Sciences, 22, 7-13. doi:10.1016/j.cobeha.2017.12.007. PMCID: PMC6095925. PMID: 30123816.
- Wang, S., Liu, H.-Y., Cheng, Y.-C., & Su, C.-H. (2021). Exercise dosage in reducing the risk of dementia development: Mode, duration, and intensity—A narrative review. International Journal of Environmental Research and Public Health, 18(24), 13331. doi:10.3390/ijerph182413331. PMCID: PMC8703896. PMID: 34948942.
- Liu, C.-C., Kanekiyo, T., Xu, H., & Bu, G. (2013). Apolipoprotein E and Alzheimer disease: risk, mechanisms, and therapy. Nature Reviews Neurology, 9(2), 106-118. doi:10.1038/nrneurol.2012.263. PMCID: PMC3726719. PMID: 23296339.
- Duan, Y., Lyu, L., & Zhan, S. (2023). Stem cell therapy for Alzheimer’s disease: A scoping review for 2017–2022. Biomedicines, 11(1), 120. doi:10.3390/biomedicines11010120.