Pancreatic Cancer Guide

80% of people with pancreatic cancer get a diagnosis too late.
Only 3-6% of diagnosed patients go on to live for five years.
More than 90% of tumors are pancreatic adenocarcinomas (PDAC).
Early diagnosis increases the chances of 5 years of living by 10.
 Where is your pancreas, and what does it do?
Where is your pancreas, and what does it do?
The pancreas is located in front of the spine and behind the stomach. It is surrounded by one of the parts of the small intestine (the duodenum), liver, and spleen. If you are interested in how big a pancreas is, imagine a leaf, about 15 centimeters (6 inches) in length.
It produces hormones to maintain blood sugar levels and generates pancreatic enzymes to digest food, which assists the body in extracting and storing energy from the food.
 What is a pancreatic tumor?
What is a pancreatic tumor?
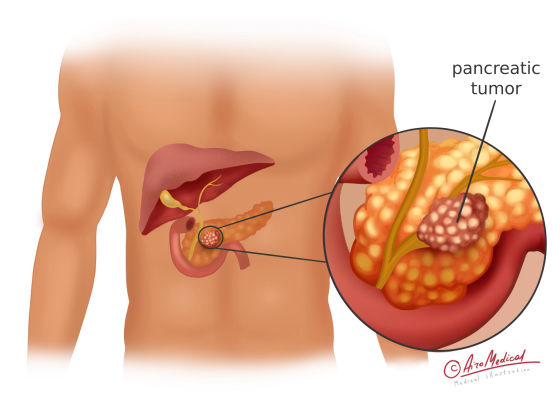 Usually, cells only divide to make new cells because the body needs them, and the body destroys old cells that are no longer working correctly. Changes in a cell's DNA can make it grow and divide out of control or stop old cells from dying when they should.
Usually, cells only divide to make new cells because the body needs them, and the body destroys old cells that are no longer working correctly. Changes in a cell's DNA can make it grow and divide out of control or stop old cells from dying when they should.
Scientists are still studying why these mutations happen and what causes pancreatic cancer. But it is recognized that they can be passed down or picked up during life. A tumor is a mass of extra cells that have grown together. Tumors can be either harmless or dangerous, or malignant.
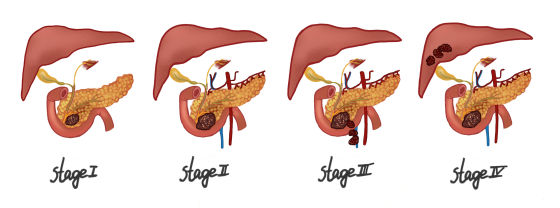
Malignant means that a tumor keeps spreading, the same as cancer. Malignant tumors are dangerous because they can spread to other organs and tissues. Metastasis is the process by which a disease spreads to other body parts. A tumor is said to be metastatic if it has spread to other body parts (it has metastasized to other locations). Doctors give cancer a stage that shows how far it has spread.
Due to pancreatic cancer pathophysiology, it can either be:
- Exocrine -- in about 95% of cases, adenocarcinoma starts in the ducts of the pancreas
- Or endocrine -- the remaining 5% are called neuroendocrine tumors, which can produce hormones.
The main issue with pancreatic cancer is that it is difficult to detect. As a result, it is diagnosed at very late stages. Pancreatic cancer accounts for about 3% of all cancer and ranks eighth among the most common cancers in women and tenth in men. Pancreatic cancer cases have increased by about 1% every year since 2000. More than 500,000 people were diagnosed with pancreatic cancer worldwide in 2021.
 Who is at risk of pancreatic neoplasm?
Who is at risk of pancreatic neoplasm?
One in 64 people will develop pancreatic cancer. Risk factors increase the likelihood of disease. If you are interested in how you get pancreatic cancer and how to avoid it, these things can raise risk:
- Smoking cigarettes, cigars, etc.
- Being overweight is also dangerous.
- Obesity-related type 2 diabetes. A normal-weight, middle-aged person who develops diabetes could have pancreatic cancer.
- Dry cleaners and metalworkers utilize chemicals.
- Chronic pancreatitis is a long-lasting inflammation and causes tumors in 5% of cases.
You can't permanently reduce danger. Men over 45 with gene mutations are at higher risk, so they must be more attentive to their health. Regular check-ups will help. Pancreatic cancer symptoms in females are not significantly different.
Can you avoid pancreatic cancer?
Indeed, we cannot avoid most cases of pancreatic cancer. The disease is more manageable if you stick to a balanced diet, avoid tobacco products, and reduce alcohol consumption, which often causes chronic pancreatitis. It is a risk factor and a family history of the disease.
 What are the signs and symptoms of pancreatic cancer?
What are the signs and symptoms of pancreatic cancer?
Most people don't show any signs in the early stages of the disease. If you ask something like “my first symptoms of pancreatic cancer,” there is no definite answer. But as the condition gets worse, people may notice the following signs:
- Eyes and skin turn yellow. It is called jaundice and appears in about 50% of pancreatic cancer patients. It has one specialty — yellowish without pain is one of the most significant symptoms.
- The color of feces and urine changes. The cause of this is the block of the liver’s bile ducts; that’s why the bile does not go to the intestine, the stool turns white like in pancreatic cancer stool pictures, and the urine opposite turns dark.
- Skin starts to itch because of a buildup of bile salts in the blood, brought on by blocked bile ducts; pancreatic cancer is responsible for the itching in this case. Also, this might lead to skin burning and general skin discomfort.
- Patients lose weight without trying, have no appetite, and always feel tired. Sometimes they feel a fever.
The signs of pancreatic cancer often look like diabetes or pancreatitis. These can be the only ones at the early stages – pain, digestive disorders, weight loss, and blood sugar-increasing symptoms like frequent urination, thirst, and dry skin.
Can pancreatic cancer be detected early?
Looking for early signs of pancreatic cancer can be challenging to detect. Since the pancreas is deep within the body, doctors can't see or feel early tumors during regular check-ups. Most people don't notice anything wrong until the cancer is vast or has developed in other body parts.
Asking a question about what pancreatic cancer symptoms is and how they can be diagnosed, you should remember, is not easy. Doctors perform screening tests or examinations to look for only certain types of malignant masses on the pancreas. In people with no signs (and who have not had such malignancy before), it can help. But in any case, for those who are at average risk of pancreatic cancer, no major professional groups recommend routine screening at this time.
 What about routine diagnostic tests?
What about routine diagnostic tests?
If the doctor thinks that the symptoms point to pancreatic cancer, they may order more tests, such as
- The results of functional liver tests and other blood tests can be used to test the pancreas and look for other standard blood markers.
- Endoscopic ultrasonography can be used to get a picture of the pancreas (EUS).
- Positron emission tomography, or PET scans, uses radioactive substances to find places that could be dangerous. After a particular dye is injected into the veins, scans of the pancreas are taken.
- An MRI scan uses magnetic fields and radio waves to take pictures of the body. It makes a detailed picture of the pancreas.
- A biopsy is a procedure in which a tiny pancreas fragment is removed and tested. After that sent to a lab for a thorough look and confirmation that the cancerous cell was there.
- Some pancreatic cancer cells regularly release proteins that can be found in the blood. Oncomarkers are the name given to these proteins.
- Newer tests that can find pancreatic cancer early may help people from families with a high risk of getting it. Most of the time, an endoscopic ultrasound or MRI is used.
For an accurate diagnosis and stage of cancer, tests may need to be done simultaneously. When the doctor gets these results, they will decide what to do next.
Where is better to go get the best treatment?
 What are the treatment methods?
What are the treatment methods?
Persons with pancreatic cancer can be treated differently, depending on the type of cancer, how far along it is, and other factors.
- Surgical resection is made when exams and tests show that it might be possible to remove all cancer. It is the best way to treat pancreatic cancer in its early stages. If the patient is diagnosed with a location that can be curable by surgery, the chances of 5-year survival increase to ten. If diagnostics demonstrate that the tumor has progressed too far to remove, palliative surgery may be performed. The goal, in this case, is not to cure cancer but to relieve pancreatic tumor symptoms or prevent problems like a blocked bile duct or intestine. To help ease digestion, a doctor can choose bypass surgery.
- Systemic chemotherapy uses drugs all over the body and kills damaged pancreatic cells. It is no matter where they are, even if there are signs that pancreatic cancer has spread. There are before and after operation chemo, or in the case of advanced tumor stage.
- Immunotherapy is a treatment that helps the body fight cancer by itself. Drugs make the immune system work better and kill sick pancreas cells. People take these drugs if their cancer starts to grow again after chemotherapy. Drugs could also be used to treat people for whom surgery can't remove cancer. It also comes back after treatment or has developed in other body parts.
- Targeted therapy is a treatment that affects only specific genes or proteins that help cancer grow. As scientists have started learning more about the changes that help pancreatic cancer cells grow, they have made new drugs that target these changes. Often they work when routine chemo drugs don't, and they often have various side effects.
- Radiation therapy is a way to treat pancreatic cancer that uses high-energy rays or particles to kill cancer cells. After surgery, oncologists may give radiation treatments to reduce the chance of cancer returning. Before surgery, radiation is given to shrink the tumor and make it easier to delete. It is suitable for tumors that are close to being able to be cut out.
Cancers that have spread beyond the pancreas and can't be removed by surgery may be treated with radiation therapy and chemotherapy. People with advanced cancer or who aren't healthy enough for other treatments like surgery may get radiation to help relieve symptoms.
Although each disease has a unique characteristic, and even in centers like the Mayo Clinic, pancreatic cancer is challenging to treat.
Which clinics fit the best?
 New treatment options
New treatment options
Scientists worldwide are trying to find new treatment methods for pancreatic cancer. The complexity of this disease is that cancer cells separate, enter the bloodstream at some point and circulate throughout the body. Therefore, the last word in pancreatic cancer treatment is:
- Transarterial chemoembolization (TACE) is a procedure that causes the least amount of damage. A chemotherapy drug is put directly into a pancreatic tumor through a blood vessel that feeds it. So, the blood vessels that nourish cancer in the pancreas are blocked (embolized) to stop blood flow and keep the chemo inside of the tumor.
- Transarterial chemoperfusion (TACP) is a method for exposing the pancreatic tumor to chemo in a local way. Cancer-feeding arteries are directly injected with chemotherapy drugs using a catheter. When a lot of the drug is inside the tumor mass, chemo kills the malignant cells.
- Radioembolization (selective internal radiation therapy with SIRT microspheres) is an internal radiation therapy that sends radioactive microparticles straight to the pancreatic tumor. Radiation spheres can kill cancer cells.
- Ablation therapy (RFA, MWA, or ethanol) uses needle electrodes to send heat to the tumor, which shrinks and kills it.
- Radiosurgery (CyberKnife, GammaKnife) is a type of radiation therapy that doesn't involve surgery. It is a unique system that uses targeted radiation to remove cancer from the pancreas.
- Proton therapy is a kind of radiation treatment. The tumor is hit with a proton with a certain amount of radiation. It doesn't hurt the healthy tissues nearby.
- Surgery is the most common way to eliminate cancer from the pancreas. The Whipple procedure is frequently used to remove malignant tumors from the head of the pancreas. Part of the digestive tract is also fixed at the same time. Distant or total pancreatectomy also can be performed.
- Robotic pancreatic surgery da Vinci uses an automated system and is less invasive. The automatic system lets doctors make more minor cuts and micro-cuts that they couldn't do with their hands before.
Pancreatic cancer can be cured if it is detected at the initial stage and treatment is started immediately.
The most qualified oncologist in pancreatic cancer
 Statistics and prognosis
Statistics and prognosis
Pancreatic cancer is the most aggressive malignant neoplasm of the digestive tract. It has an unfavorable prognosis due to its late diagnosis. Due to the American Cancer Society, only about 23% of patients survive another year after the diagnosis. However, about 8.2% are alive five years after the diagnosis.
If the cancer is found early enough to be removed by surgery, 42% of people will still be alive after five years. Sadly, only about 13% of people are diagnosed at this point. The average time a person with pancreatic cancer lives is 3 to 3.5 years if identified before the neoplasm spreads, the
If cancer has spread to nearby structures, only 14% of people will still be alive after five years. 52% of those diagnosed with cancer after its spread have only a 3% chance of living for five years.
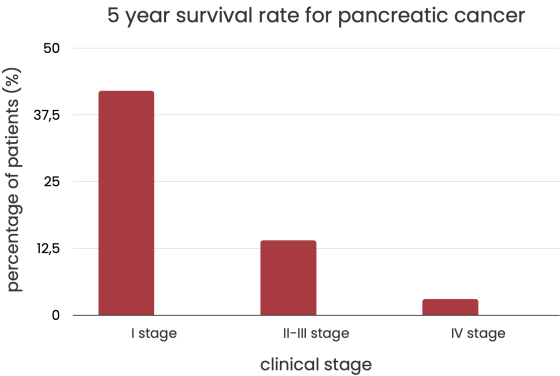
Good news: recent studies that came out in 2020 showed that patients with tumors found at the earliest stage IA (less than 2 cm) can have a five-year survival rate of over 80%. Studies performed in 2015 claim that the numbers were twice lower.
Survival depends on various things, and no two cases are the same. Only by taking a unique approach to each patient and choosing the right treatment plan is it possible to recover or improve the quality of life.
References:
- American Cancer Society: if You Have Pancreatic Cancer
- NHS: What is pancreatic cancer?
- WebMD: Pancreatic Cancer
- Cancer Research UK: Together, we will beat cancer
- American Society of Clinical Oncology (ASCO): Pancreatic Cancer: Statistics
- John Hopkins Medicine: Pancreatic cancer prognosis
- Frontiers' social media: Role of Radiofrequency Ablation in the Management of Unresectable Pancreatic Cancer
- BioMed Central Ltd unless otherwise stated: Robotic and laparoscopic surgery of the pancreas: a historical review